The winter months are here! For those of us who live or work in in a cold climate, some form of heat is on, the windows are closed, and we may be sneezing and wheezing.
Analytically-minded engineers are undoubtedly asking how they can design and manage HVAC systems to mitigate winter-time dry skin, chapped lips, colds, and asthma flare-ups. First, we need to understand the causes of these symptoms. Dry skin is easy to understand, but allergy-related illnesses such as asthma are more confusing. Asthma “attacks” have many triggers, such as exercising in cold temperature, contracting a viral illness, and most commonly — inhaling an allergen; a particle which the person is sensitized to from prior exposure.
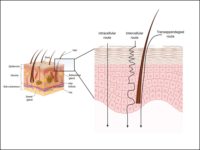
Our immune system has the difficult task of defending our external borders, namely skin surface area (for adults 1.5 to 2 m2) and lung surface area (50 to 75 m2). Protection of these surface areas by resisting penetration by harmful gases, liquids, drugs, microbes, and pollutants is challenging, especially for the delicate airway tissues. The protective task includes the identification and recognition of friendly versus harmful intruders on the mucus membrane border. When a pathogen is detected as harmful, appropriate countermeasures have to be activated.
In the first years of a child’s life, the immune system is flexible and capable of learning. If the developmental window of this learning period is missed, however, wrong identification and categorization decisions are difficult to retrain. We will see later in this article that this has serious consequences for a lifetime.
The number of people with asthma in Westernized countries has doubled in the last several decades and now affects over 24 million people in the U.S. alone. Can increased wheezing in the winter, therefore, be attributed to high levels of indoor dust combined with dander from people and animals carrying microorganisms, allergens, and skin flakes as well as mite, pollen, and other organic allergens penetrating our houses by air, shoe soles, or pet paws?
Good Dust and Bad Dust
A fascinating “experiment of nature” has been discovered in rural communities from Germany to Russia to Amish communities in the U.S. Children who are surrounded by animals and barn dust during their early years, paradoxically, have far less asthma than children living in more “hygienic” conditions! The protective effects are strongest when children are raised with frequent and close contact with animals on traditional farms.
Is there a magic ingredient in the barn dust? Apparently there is! It’s the abundance of microorganisms and animal allergens in the dust, which can be measured and expressed quantitatively as the endotoxin or allergen load. When children around 10 years old, brought up in urban or rural environments, are exposed to different loads of endotoxins and allergens their bronchi respond in different patterns. A high percentage of children from rural areas show no or little asthma reaction, while some of the children from urban areas have an asthma attacks triggered by small loads of endotoxins and allergens. What makes them respond differently?
Children brought up in urban environments, with exaggerated hygiene, may miss healthy exposure to allergens and microbes needed to train an efficient, adult immune defense system. With this training, wrong decisions by the border control of mucus membranes can lead to false allergic alarms and impaired defense reactions to microbes later in life.
Studies indicate that for optimal functioning of immune processes in mucus membranes, a proper water content of mucus- and cilia-layers is mandatory. When animal-related microbe particles, such as endotoxin and allergens, land on well-hydrated mucus lined airway passages in early life, developing immune cells categorize the ubiquitous molecules as safe or harmful and will recognize them appropriately in the future. ES