Once upon a time, humans lived outdoors in harmony with vast and diverse populations of bacteria, fungi, and viruses, largely unaware of the presence of these microbes.
As ever-curious humans, however, we eventually created magnifying lenses to see more than our naked eyes were capable of. In the 1500s, tiny moving “germs” were spotted in pus oozing from infections, so we gladly blamed diseases on these microbes. This was a relief because we could now theoretically control devastating human losses from cholera and the “Black Death” plague. By 1880, the germ theory of disease was widely accepted, and our war against microbes was energetically underway. By the 1940s, we had created the first flu vaccine, and the first antibiotic, penicillin, was being produced in mass. The 1962 Nobel Prize winner in medicine boldly (and incorrectly) stated, “To write about infectious diseases is almost to write of something that has passed into history.”
Meanwhile, building materials and techniques became more sophisticated. After WWII, transportation allowed distant shipping of less expensive materials for the rapid construction of homes and industrial and commercial buildings with architectural and HVAC designs that were non-specific to climate zones. Previous vernacular designs once suited to local geographies were largely replaced by this universal, light material construction.
As humans leaned more and more on social and economic hierarchies to define our value, we displayed our success and power through beautiful buildings with large windows and warm interiors. In 1970, the oil embargo and subsequent energy crisis led building designers to make buildings more airtight with energy-efficient ventilation using less outdoor air and increased recirculation of interior air. Currently, most urban buildings are tightly sealed with non-operable windows, comfortable indoor temperatures, and very low indoor humidity levels that are non-detectable to humans.
Now, medical professionals are seeing an increase in infections from both new and re-emerging bacteria and viruses as well as more chronic inflammatory and auto-immune disorders. Despite our medical armamentarium, we are still losing our battle against rapidly evolving pathogenic viruses and resistant bacteria that we’ve been fighting since the beginning of our move to indoor living. Over the past 30 years, a new infectious disease has emerged every year, with the total number more than tripling since the 1980s.
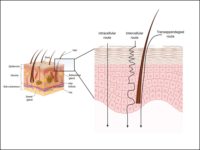
Big surprises came starting in the early 2000s, when new testing techniques provided a closer look at our bodies and environments. We now know that bacteria, viruses, and fungi — those tiny organisms that we had labelled as bad germs and tried to eradicate — are actually all around us; they’re on our skin, in our digestive tracts, and even in our lungs. Perhaps the most surprising finding is that the presence of most of these microbes improves our health. It’s usually when we disrupt their diverse and balanced communities with antibiotics and sterilization attempts that we get sick.
So, now what do we do? Should we continue to kill bacteria? How can we coexist with these “bugs” without succumbing to overwhelming infections?
First, we must realize that all bacteria, viruses, and fungi are not bad germs. We must learn to live with the good micro-organisms while still protecting ourselves from pathogens. When our immune systems or natural skin and membrane barriers are seriously impaired, such as when we are on the operating table or without immune cells right after a bone marrow transplant, it’s best to stay away from all bacteria and viruses. The rest of the time, even when we are patients in the hospital, complete eradication of all microbes is overkill.
What does this mean behaviorally? While hand gel is appropriate in the hospital, do we need to carry it on our belts so we can douse our hands every five minutes? Probably not. Should we let our children play in the soil? Yes. Should we cuddle in our beds with canine pets? Yes.
What does this revolution of knowledge tell us about building management?
-
We need to stop managing indoor air in a way that preferentially selects the pathogenic bacteria and viruses. A starting place is to try to achieve indoor water vapor levels of 40-60 percent rh, a zone known to decrease the infectivity of many viruses and bacteria while simultaneously hydrating our natural mucus membranes.
-
Instead of cleaning with powerful bactericidal solutions, we should re-establish diverse communities of microbes with probiotic solutions.
-
When building spaces accumulate mold, dust, or other layers of “crud,” the first step is to do the hard and unpleasant work of removing the biomass. Robotic misting or short-wavelength light zapping to eradicate all microbes should be saved for physical spaces with the most vulnerable patients, such as bone marrow transplant units or for laboratory hoods, where experiments are done with known lethal pathogens.
For centuries, humans have witnessed the amazing capacity of microbes to mutate, exploiting our narrow-minded attempts to eradicate them by increasing their virulence and ability to infect us. We must now learn to respectfully cohabitate with good microbes, recognizing that we depend on them for our health.