COMMON CONTAMINANTS IN HEALTH CARE FACILITIES
GUIDELINES AND CODES AFFECTING IAQ IN HOSPITALS
- Implementing IAQ measures such as outdoor air delivery monitoring, which ensures that the facility achieves prescribed outside ventilation rates during its operation.
- Increasing outside air ventilation rates by 30% above ASHRAE 62.1-2007, which allows for further dilution of the indoor pollutants.
- Developing and implementing a construction IAQ management plan before building occupancy, which is used to evacuate the air-borne contaminants that were collected in the building during construction; and the reduction in the use of contaminants that are odorous, harmful, irritating and/or harmful such as VOC and urea-formaldehyde by documenting the use of construction and furnishing materials with low or no levels of certain chemicals known to cause harm.
IAQ CONSIDERATION IN HVAC DESIGN
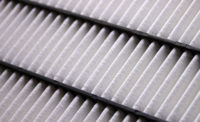
- Outdoor air minimum ventilation requirements and air change requirements for each space. These design criteria address the dilution and removal of contamination such as fungal spores, bacteria, viruses, pollens, and other hazardous chemicals.
- Pollutant source control inside and outside of the hospital. These requirements will be met by proper filtration specification and the design of the exhaust system to remove contaminants from within the facility.
- The system’s ability to restrict air movement between certain rooms and departments. This will be addressed by the pressure rela-tionship requirements to limit the movement of contaminated air from one area to the other.
- Specification of means to ensure that the system is functioning as designed.
- Ensure that an accurate airflow monitoring station is installed in the outside air intake; specify accuracy of plus or minus two percent (+/- 2%) of reading at plus or minus a quarter percent repeatability (+/- 0.25%). In my experience, the Ebtron Gold series is one of the best available in the industry because of its accuracy and ease of installation in locations where most traditional technologies cannot be applied. The control specification should include analogue input points with maintenance alarm, DDC control point, setpoint adjustment, alarm limits, and trending.
- Ensure than an accurate magnehelic pressure gauge is specified. Dwyer series 2000 is a very accurate one that is used by most air-handling unit manufacturers. The control specification should include an analogue input point with maintenance alarm at the BAS workstation.
- Room pressure monitors should be specified for specialized areas such as operating rooms, procedure rooms, isolation rooms, and pharmacy IV preparatory rooms. These rooms should be designed to maintain a differential of 0.0015 in of water between adjacent communicating spaces. These pressure monitors should include an audible alarm as well as a maintenance alarm at the BAS when the rooms are not maintaining the design pressure differential. Upper and lower limits of pressure should be specified in order to avoid nuisance alarms.
CONTROLLING IAQ DURING BUILDING OPERATION
CONTROLLING IAQ DURING RENOVATION PROJECTS
- The project’s impact on the health care environment
- The highest-risk patients and areas
- The need for and placement of barriers for airborne contaminants, as well as specialized ventilation and/or filtering
- Entry and exit for workers and materials
- Work schedules and the time of day appropriate for construction
- The need for humidity and temperature control, noise suppression, and vibration dampening and personal protective equipment (PPE), as well as the type of PPE needed
- Air handling and ventilation in specially designed areas, the potential need for additional isolation rooms and limiting of waterborne pathogens in the water system
- Depressurizing the renovation work area in relation to the adjacent spaces to prevent the exfiltration of construction dust to adjacent spaces
- Ensuring that negative pressure is maintained in the renovation areas by using pressure monitors