In health care facilities, HVAC systems are designed to perform several tasks. They purify the air; cool, humidify, dehumidify, and pressurize the space; and exhaust air from the facility. The combination of these tasks immensely affects IAQ in the health care setting. If the outside air is not properly filtered, excessive dust from the outdoors is drawn into the building, which may result in poor IAQ. If the supplied air to the clinical spaces is not conditioned or heated satisfactorily, the hospital patients, staff, and visitors will experience thermal discomfort.
The concept of IAQ is especially important regarding the environments within health care facilities. The patients within the health care facility and the staff are all directly impacted by the quality of air in the building. An optimal health care space is one that enhances patients’ comfort and healing. IAQ plays an important role in this. Since 2012, patients’ comfort has also been tied to the Center for Medicare and Medicaid Services’ (CMS) rating system and Hospital Consumer Assessment of Health Care Providers and Systems (HCAHPS) via patient surveys. These patient satisfaction surveys have resulted in many health care facilities being more vigilant in ensuring their facilities have better IAQ and reduced nosocomial infections.
The comfort of the staff members in a health care facility is also important to ensure their performance is not affected by poor indoor environmental conditions. Staff for these health care facilities is comprised of the doctors, nurses, housekeeping, facilities maintenance, administration, etc.
Air-handling units, the most common means of air distribution in health care buildings, are used to provide the airflow required for ventilation, heating, cooling, humidification, and infection control. They also provide the required air changes, filtration, and ventilation to minimize the spread of airborne infectious diseases. If supplied air to the clinical spaces is not properly dehumidified or humidified, this may promote microbial growth on the interior surfaces and also affect health care acquired infections.
GUIDELINES AND STANDARDS FOR IAQ IN HEALTH CARE FACILITIES
ANSI/ASHRAE Standard 62.1 - 2019, “Ventilation for Acceptable Indoor Air Quality,” is a recognized industry engineering design standard that directly addresses IAQ. This standard is also referenced by LEED rating systems. The standard addresses the criteria for comfort, which include air temperature, relative humidity, contaminants, air distribution systems, and pressurization. It also includes requirements specifically identified for health care occupancies but refers to ASHRAE 170 for ventilation requirements.
ASHRAE Standard 170, “Ventilation of Health Care Facilities,” which was first published in 2008 and is currently in its 2017 revision, was specifically created for the health care environment. This standard is Part 3 of the Facilities Guideline Institute’s (FGI’s) Guidelines for Design and Construction of Hospitals, 2018. The standard goes into greater detail than ASHRAE Standard 62.1 as it relates to the health care environment. It provides design standards on filtration, air movement, ventilation, air temperature, humidity, and pressurization for various health care-specific spaces. Health care facilities must, at a minimum, comply with ASHRAE 170 and other regulatory standards with respect to air change rates, humidity requirements, diffuser types, and pressurization.
In order to qualify for Medicare and Medicaid reimbursement, CMS requires that health care facilities meet the requirements established by National Fire Protection Association (NFPA) 101, Life Safety Code - 2012. NFPA 101 includes, by reference, additional NFPA Standards: NFPA 90A, “Standard for the Installation of Air-Conditioning and Ventilating Systems,” and NFPA 99, “Health Care Facilities Code.” These are just two relevant standard examples. Most facilities will meet the requirements of these codes to meet the conditions of participation (COP) of CMS.
The U.S. Centers for Disease Control and Prevention (CDC) has many established policies and procedures for the operation of health care facilities. It also offers documents such as Guidelines for Environmental Infection Control in Health Care Facilities (2003), which was updated in July 2019, which offers direction on how to prevent or minimize chemical, biological, and radiological contaminants from impacting the facility’s ventilation systems. Since health care facilities are referred to as “defend-in-place” occupancies, the safety and quality of the indoor environment becomes paramount in many operational environments.
DESIGNING FOR IAQ IN HEALTH CARE FACILITIES
There are four criteria that should be considered when designing for IAQ in health care settings: the patients, staff, the building, and the building’s external environment. Each of these criteria should be addressed individually in order to design for optimal IAQ.
The COVID-19 pandemic demonstrated the importance of having stringent IAQ within a hospital environment. Patients who are infected with the virus and are being treated, if not contained in a separate cohort, can infect hospital staff and other patients. The effectivity of air distribution systems stood its test and was one of the major concerns for most hospitals during the first COVID-19 surge. Most hospital systems worked with their design engineers to assess which air-handling units could be modified into single-pass systems. Where there is possibility for this operation, the facilities team will modify the air-handling unit’s operation to be 100% outside air with the return air fully exhausted. This method of operation is one of the safeguards that allows the space to remove most of the contaminants that are captured in the airflow system to be expelled to the exterior. Care was taken to ensure this exhaust air was run through HEPA filters before it was dispersed to its surroundings. This precaution was taken because there is not enough known about the aerosolized characteristics of the COVID-19 virus.
AIRBORNE INFECTION ISOLATION (AII) ROOMS
Airborne infection isolation (AII) rooms have been the most sought-after spaces since the onset of the COVID-19 pandemic. AII rooms are used to protect patient and staff from any impact patients can have on their external environments. AII rooms are negative pressure rooms used to contain airborne contaminants in a hospital. Viruses, bacteria, fungi, yeasts, molds, pollens, gases, volatile organic compounds (VOCs), small particles, and chemicals are part of a larger list of airborne pathogens that can be found in a hospital environment. If AII rooms are not properly pressurized, this will pose a risk of airborne transmission of pathogenic bacteria and viruses. This room is designed to exhaust more air than is supplied. Typically, about a 20% differential is used to ensure internal air flows directionally from the ante room and adjacent corridor, which affects the IAQ of the space. If these spaces are not designed and constructed properly, they will expose hospital occupants to the airborne pathogens and inevitably result in nosocomial infection.
These rooms are very important because they are the best rooms to perform intubation of COVID-19 infected patients before they are placed on ventilators. During the process, a tube is inserted into the lungs, which sometimes will cause fluids to be dispersed in the direction of the health care providers. This fluid may contain contaminants that can become airborne. Having the procedure done in these rooms will ensure the airborne contaminants are exhausted to the outside through HEPA filters and will not affect the other occupants in the hospital.
PROTECTED ENVIRONMENT (PE) ROOMS
PE rooms are designed to be positively pressurized with respect to the corridors and ante rooms (if designed with one). If PE rooms are not properly pressurized, they will pose a risk to the patients that are receiving treatment. Patients in these rooms have compromised immune systems and therefore need to be protected from the impact of the surrounding hospital environments. These rooms are designed to supply more air than is exhausted; typically, about a 20% differential is necessary to ensure an external direction flow of air from the room.
OPERATING ROOMS (ORS)
In ORs, both the patients and the staff must be protected by the HVAC system. IAQ in operating rooms are of extreme importance because the environment should be sterile for surgical procedures. This room is particularly important because some procedures are invasive and will expose the inside of a patient’s body cavity to the surrounding environment of the surgery room. These rooms are designed to be positive pressure with respect to the adjacent corridor. Airborne pathogens can infiltrate the internal body cavity during surgery and are often responsible for a lot of nosocomial infections.
ORs are also designed to have lower space temperatures than other areas in the hospital and are required to operate between 20%-60% RH. ANSI/ASHRAE/ASHE Standard 170 - 2017, “Ventilation of Health Care Facilities,” recommends a temperature band of between 68°-75°F; however, the guideline also states that surgeons may require lower temperatures. Most ORs are operated at a much lower temperature than 68° to cater to the comfort of the surgeons. Sometimes these ORs are designed to have set point temperatures as low as 62°.
The air distribution devices in the ORs are very important for keeping patients and staff comfortable but also to ensure the airflow pattern is unidirectional and does not allow mixing around the operating table. Laminar diffuser patterns are used to achieve this; they are designed to provide uniform, unidirectional, low-velocity airflow over the patients. The downward pattern displaces airborne particulate down and away from the operating table and toward the low return level diffuser. The minimum air change rate stipulated by ASHRAE 170 for ORs is 20 air changes per hour (ACH). The higher the air change, the cleaner the space, and the better the IAQ.
METHODS TO MAXIMIZE IAQ
IAQ is really looking at the quality of the air that is distributed through the health care facility. The cleaner the air, the better it is for the patients and staff. In the design of health care spaces, all the required IAQ codes and guidelines need to be considered, and the more stringent codes should be followed. When designing the system for a health care facility, engineers need to examine the entire path of the air from the intake to the diffuser or grilles in the space. Additionally, they need to examine the airflow through the health care spaces and its route back to the air-handling units via the return ducts or outside through exhaust ducts. Any contaminants that are in the air path must be identified, and measures must be employed to remove said contaminants. Care must be taken to prevent untreated air from entering the facility.
The path the outside air takes through health care facilities starts at the point where it enters the building through the intake louvers. Air intakes should be located to prevent contaminants from being drawn in from air exhaust and other pollutant sources. ASHRAE 170 standards and other codes dictate minimum distances from vehicle traffic and building exhaust. It’s very important to note that these minimums don’t take into account site specific conditions and design details, such as building geometry, and external conditions, such as prevailing winds. These conditions may necessitate a greater separation than the code requires. Emergency generator exhaust could be 200 feet away from an intake, but if the wind and elevations are just right, the fumes could still be drawn into an air intake. Care must be taken to analyze the location and configuration of the air distribution system’s outdoor air intakes to minimize the chances for cross contamination.
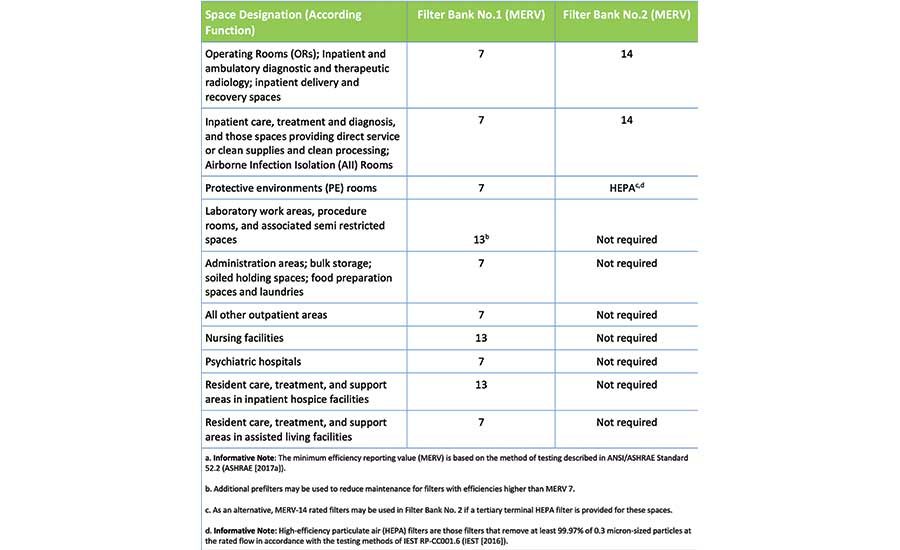
Once the outdoor air is drawn into the health care facility, it needs to be filtered. ASHRAE 170 provides the minimum requirements for filtration based on what health care spaces are being served by the system, see Table 1.
There are several types of filters to consider. Particulate filters are rated in terms of efficiency with a minimum efficiency reporting value (MERV). MERV ratings, as established in ASHRAE Standard 52.2, “Method of Testing General Ventilation Air-Cleaning Devices for Removal Efficiency by Particle Size,” range from the lowest efficiency at 1 to the highest efficiency at 16. Filters with a MERV rating of 1 are based on retaining most penetrating particle size (MPPS) of 10 microns (dust and pollens), while filters with a MERV rating of 16 are based on a filter’s efficiency at the MPPS of 0.3 microns (smoke, viruses, and bacteria).
HEPA air filters and ultra-low particulate arrestance (ULPA) air filters have efficiencies even greater than those identified in ASHRAE Standard 52.2 and are given MERV ratings in the 16-20 range. HEPA filters are 99.97% based on retaining MPPS of 0.3 microns in size, and ULPA filters are 99.999%, retaining MPPS 0.02 microns in size. Particulate filters are typically provided in pleated media, bag, and cartridge types. In critical spaces, filters are not just used in the air-handling equipment, but also at supply diffusers or grilles, which are the point of air delivery to the space, where they act as the last line of defense to keep contaminants from entering the health care space.
With this description of particle size, there is a misconception that HEPA filters do not remove particles smaller than 0.3 micron. This is not the case because HEPA does not act like a strainer where particles above a certain size are not able to pass through, but rather they use four different filtration mechanisms to effectively trap particles of varying sizes (sizes both larger and smaller than 0.3 microns). The HEPA filter will remove at least 99.97% of dust, pollen, mold, bacteria, and any other airborne particle with a size of 0.3 microns. The diameter specification of 0.3 microns responds to the worst-case MPPS. Particles that are larger or smaller are trapped at an even higher efficiency. Most of the small particles, like a COVID-19 size (0.11 microns) virus, can be captured by HEPA and ULPA filters.
Gas-phase filtration utilizes chemical filters that can be used to minimize contaminants from entering the health care spaces. The most common types of gas-phase filters use either activated carbon or potassium permanganate (often referred to as “purple pellets”). Consider the use of gas-phase filters when it is impossible or impractical to locate intakes sufficiently away from irritating, corrosive, or odorous airborne contaminants. This can be used for intakes that are located near helicopter plumes.
Electronic air filtration is used to minimize contaminants from entering the health care environment. Electronic air filters typically incorporate charged plates or wires and electrostatically charged particles as they pass to aid in arresting the conveyance of the particles. This type of filter generally works best on particles that are less than 10 microns in size. Electronic filters that incorporate charged plates do not require regular media replacement but do require regular cleaning. Electronic filters that incorporate charged wires still require particulate filters but because of the charge, the filter life is extended due to the charge’s impact on arrestance efficiency.
Ultraviolet (UV) disinfection can be used as a supplemental air disinfectant method in hospitals for the prevention and spread of tuberculosis. There are three primary methods used in the health care industry: duct radiation (UV in air-handling units), upper room air radiation (UV mounted in ceilings and protected from the bottom to prevent human exposure), and stand-alone units (self-contained UV shielded units containing a variable number of bulbs).
UV germicidal irradiation (UVGI) can be used in a central HVAC system to augment but not replace HEPA filtration, according to the 2003 CDC guidelines. UVGI can be used in this setting if risk assessment indicates that supplemental engineering controls are needed. The benefits of UV disinfection of airflow are still in question because the industry is not convinced it will reduce infection beyond the level provided by HEPA filtration. For pathogens, such as Aspergillus and Staphylococci, UVGI can be effective in reducing airborne pathogens when combined with filtration, but there are limited data showing efficacy in reducing infection risk. Several manufacturers have published material about the effectiveness of UV-C lamps at the right doses in deactivating the COVID-19 virus. The use of UVGI in a health care setting should be further investigated to ensure it can actually reduce the occurrence of airborne infection, and, therefore, justify the expense.
UVGI can also be installed near ceilings to irradiate upper room air in ORs; this method can also be an effective strategy to augment the performance of HVAC systems by increasing filter efficacy and efficiency through controlling the growth of biofilm on filters. Some evidence supports upper-room UVGI as an effective means for deactivating bacteria and virus.
HUMIDIFICATION AND DEHUMIDIFICATION
Humidity is an important component metric for IAQ. ASHRAE 170 contains guidelines about minimum and maximum humidity levels in all the spaces in the health setting. Humidity levels are important for the overall comfort of patients and staff, but it is even more significant for critical spaces.
For cold climates, additional means of humidification may be necessary to maintain the recommended minimum relative humidity levels in various health care spaces per ASHRAE 170. In colder climates, humidification must be added to the airstream to compensate for the lack of moisture. To add humidification, isothermal steam injection is typically preferred in health care applications, but adiabatic steam humidification is now allowed for hospitals. It is recommended that clean steam free of amines be used for humidification because the steam is injected directly into the airstream.
The location of any type of humidifier in the air distribution system in the hospital should be carefully evaluated to ensure the discharge of the humidifiers does not condense on any of the system’s filter media. The absorption distance should be a key factor when designing humidification systems. The absorption distance is the linear length of air travel that it takes for the steam to be fully absorbed into the airstream. The humidifier should be installed in straight, unobstructed duct to fully encompass the absorption distance.
For warm and humid climates, dehumidification will be necessary to maintain the recommended maximum relative humidity levels in various health care spaces per ASHRAE 170. Therefore, means of dehumidification must be implemented to meet the design standards and the comfort of staff and patients.
The standard health care dehumidification method is to subcool the airstream to maximize condensation (moisture extraction) and then reheat the air to achieve the desired supply air temperature to the space. Another method of doing dehumidification for more critical spaces, such as ORs and pharmacies, is to introduce some sort of desiccant into the airstream. A desiccant wheel will allow the humid airstream to pass over the desiccant and will extract the moisture in the process.
AIR DISTRIBUTION
After the air is passed through the air-handling units and filtered, sanitized via UVGI, heated or cooled to the design supply temperature, and humidified or dehumidified depending on the season, it must be distributed to the various spaces in the health care facility. ASHRAE 170-2017 will dictate the minimum outside and total ACHs required for each health care space in order to ensure good IAQ. For example, ER waiting rooms must have a minimum of 2 ACH of fresh-air ventilation and 12 ACH of total air movement, and the space is required to be negative pressure with respect to the adjacent spaces. ORs must have a minimum of 4 ACH of fresh-air ventilation and 20 ACH of total air movement, and the space is required to be positive pressure with respect to the adjacent spaces.
CONCLUSION
IAQ is of the utmost importance in the design of a health care facility. The comfort of hospital patients, staff, and visitors is directly related to the internal environmental conditions. IAQ is also linked to infection control because of the role it plays in minimizing airborne infection. While the quantity of air distributed to the space is important from an air quality standpoint, space pressurization is perhaps even more important for critical hospital spaces. Designers must be certain the air quantities are balanced so that air travels from the cleanest spaces — critical spaces, such as intensive care units (ICU), ORs, and neonatal intensive care units (NICU) — to the dirtiest spaces — noncritical spaces, such as soiled utility and decontamination rooms. Designers need to ensure outside air that is brought into the health care facility is properly filtered, maintained within specific parameters for temperature and humidity, and not allowed to contaminate other clinical spaces as it is routed back through the return system.