Mechanical ventilation systems are key mechanisms for controlling airborne infection in health care environments, and the importance of these systems has come to the forefront during the COVID-19 pandemic. The goals of mechanical ventilation systems in hospitals are to replace contaminated air with clean air, minimize the mixing of dirty and clean air, regulate ambient temperature and humidity, and maintain pressurization relationship to adjacent spaces. There is little consensus that ventilation systems play a key role in minimizing the spread of airborne diseases in hospitals. The ventilation requirements for health care spaces are stipulated by the ANSI/ASHRAE/ASHE Standard 170, “Ventilation of Health Care Facilities.” This standard defines the minimum outside air, minimum total air change rate, minimum exhaust, and pressure relationship to adjacent areas. The efficacy of the ventilation system in the hospital environment is highly dependent on the amount of outside air supplied, air change rate, and air filtration system. There are other contributing factors that can impact the effectiveness of a ventilation system in health care spaces, such as lack of proper filter routine maintenance, high levels of contaminants in the outside air, and locally polluting activities in the indoor space.
NOVEL CORONAVIRUS (COVID-19)
A virus is a small infectious agent that can replicate only inside the living cells of organisms. Most viruses are too small to be seen directly with a light microscope. Viruses infect all types of organisms, from animals and plants to bacteria. The most important virus in the current pandemic is the novel coronavirus known as COVID-19. This is a new coronavirus that had not yet been previously identified. This is not like other coronaviruses that commonly circulate among animals. Coronaviruses from animals rarely affect humans; however, there are many types of coronaviruses in humans that usually cause mild respiratory illness.
The COVID-19 virus is thought to spread mainly between people who are in close contact with one another through respiratory droplets produced when an infected person coughs, sneezes, or talks. The main route of transmission is through droplets, or smidgen of liquid, mostly via sneezing or coughing.
These droplets can land in the mouths or noses of people who are nearby or may be inhaled. On March 16, the World Health Organization (WHO) dispersed an “airborne precaution” for medical staff after a study showed the coronavirus can survive in the air in some settings. The study showed the coronavirus can go airborne and stay in the air depending on the environmental properties of the air.
THE ROLE OF VENTILATION IN MINIMIZING COVID-19 SPREAD
Ventilation systems are important mechanisms to help minimize the spread of COVID-19 in hospital settings. A ventilation system helps by removing the virus through air filtration and enhancing air change rates, air compartmentalization, and source control.
One of the biggest challenges facing a hospital engineering facilities team is to figure out how they can modify existing hospital ventilation systems, temporary or long term, to help to minimize the spread of COVID-19 through the air system.
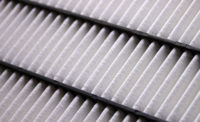
Ventilation supply varies from space to space within the hospital. Some hospitals use 100% outside air system designs, but many air distribution systems in hospitals include a mixture of outside and recirculated air. This mixed air is passed through a filtration system to remove airborne contaminants.
During this pandemic, engineered systems played a vital role in limiting the transmission of COVID-19 in hospitals. The first level of defense for the health care staff is personal protective equipment (PPE), but the value of the appropriate ventilation system should not be underestimated. An enhanced mechanical ventilation system will help minimize the recirculation of contaminated air in a hospital’s air distribution system. Many of the hospital systems used increased ventilation as a means of minimizing the recirculation of air within the hospital during the first pandemic surge. They modified the air-handling units (AHUs) to operate at 100% outside air or full economizer mode. This is for AHUs that have the capability of operating in this manner; some units were not designed to operate in full economizer mode. Doing this would have limited the path of the airborne spread of the virus if it had the capabilities of being aerosolized and travelled for long distances in the airstream. While the behavior of the virus in this manner is still under investigation, facilities teams need to act to first “do no harm” until the full behavior of the virus is thoroughly understood.
The first pandemic surge occurred during the spring and winter months, which meant the cooling capacity of these AHUs could handle the limited amount of required cooling. It has been reported that most hospitals had to convert their AHUs back to normal operation since the start of summer because the cooling coils in the units were not sized to operate at 100% outside air in the humid summer months. For future pandemic occurrences, health care facilities will need to upgrade the capacity of the cooling coils in their AHUs and size the coils in any new AHUs to be able to operate at 100% outside air all year-round if the need arises.
The ventilation system for all health care facilities have been placed under a microscope during this pandemic because people see these systems as part of the key mechanism of minimizing the spread of COVID-19. During the first pandemic surge and country lockdown, many health care facilities shut down elective surgery in order to concentrate on treating the COVID-19 infected patients. This is not the case for most health care facilities since the reopening of most states. We now have a situation where health care facilities are treating multiple patients, including some that are COVID-19 infected. WSP engineers have been working with many health care facilities to modify their existing ventilation systems so that they can be more prepared to handle both COVID and non COVID patients.
EXHAUST AIR
Exhaust air is a very important part of ventilation systems in hospital settings. The minimum exhaust requirements for health care facilities are also stipulated by the ANSI/ASHRAE/ASHE Standard 170. The exhaust from airborne infection isolation (AII) rooms, bronchoscopy and sputum collection rooms, pentamidine administration rooms, emergency department public waiting areas, nuclear medicine hot labs, radiology waiting rooms for patients with respiratory diseases, pharmacy hazardous-drug exhaust enclosures, and laboratory work area chemical fume hoods needs to be discharged outside of the hospital to prevent contaminated air from being recirculated or entrained back into the building air intake. The exhaust outlets from these areas, except for laboratory chemical fume hoods, should be arranged to be discharged in the atmosphere at a minimum vertical height of 10 feet.
Laboratory chemical fume hoods are required to be discharged with a minimum stack velocity of 2,500 feet per minute (fpm), which is usually achieved by using high plume dilution fans. Routing your exhaust from the hospital is of extreme importance. Exhaust louvers that carry contaminated exhaust air should be designed to be located 25 feet from the nearest outdoor intake, openable windows/doors, and public areas. The removal of COVID-19-related airflow contaminants from every room is very important in protecting hospital staff and patients.
During the COVID-19 pandemic, there was a rush to create negative isolation rooms to house COVID-19 patients (see Figure 1). These rooms were created by adding exhaust to existing patient rooms and ensuring the exhaust airflow from these rooms was higher than the supply air to the room.

FIGURE 1. Temporary negative-pressure rooms for COVID-19 patients.
Many infected patients were moved to these negative-pressure patient rooms. The negative-pressure rooms were deployed to help prevent the spread of COVID-19 from an infected patient to other persons in the hospital. Some of these rooms were medical-surgical patient rooms that were modified to have a negative pressure relationship to the adjacent corridors to prevent an aerosolized COVID-19 virus from migrating to other areas in the hospital. The exhaust from these rooms was often routed through high-efficiency particulate air (HEPA) filtration before being discharged to the outside of the building. Installation of HEPA filters in the air exhaust stream will ensure the air is filtered to a high standard and will not pose any harm to the surrounding areas of the hospital. This is also important to ensure contaminated exhaust air is not entrained in air intake louvers. It is important to utilize bag-in, bag-out HEPA filters in order to protect facility engineers from contacting contaminants when replacing the filter media.
These modified negative pressure rooms should not be confused with true AII rooms because they don’t meet the minimum requirements stipulated by the Facility Guidelines Institute (FGI) Guidelines for Design and Construction of Hospitals, 2018. AII rooms are required to be well-sealed to prevent excess air leakage into or out of the room. Because of this, they have to be constructed to certain specifications. These rooms have much higher air change rates than medical-surgical patient rooms — they have an ante room separating them from corridors and should contain a permanent visual pressure differential monitor to visually show that the room is maintaining negative pressure to the corridors and ante rooms. These modified patient rooms were not built to these specifications, and the modifications for the pandemic were deemed temporary, so, therefore, there was no need to renovate to the full AII specification. However, it is important to note that many negative isolation rooms were created throughout the country to help with COVID-19 patient treatment. These rooms were not only created in hospitals, they were constructed in convention centers, hotels, shipping containers, etc.
RECIRCULATED AIR (RETURN)
Recirculated or return air — air that is routed back to the AHUs before it is filtered, conditioned, and returned to the space — is a very important part of the ventilation air in a hospital. Recirculation by in-room units is not allowed in most of the critical spaces within a hospital, and, therefore, units, like fan coil units, VRV units, chilled beams, induction units, etc., are not allowed within critical spaces.
The quality of this recirculated air is very important in maintaining a ventilation system’s effectiveness within health care settings. This air is also important to minimize hospitals’ energy use so that these facilities can meet ASHRAE 90.1 energy guidelines. During the pandemic, air recirculated from areas that housed cohorts of infected COVID-19 patients was not allowed to return to the AHUs that served other areas. Many facilities added HEPA fan units to intercept the return path within the ductwork and discharged the return air outside of the hospital. In those cases, the return air became exhaust (Figure 2).

FIGURE 2. A purge mode system.
PANDEMIC VENTILATION DESIGN
The ventilation design for hospitals will need to be revisited to ensure these systems may be easily modified to meet future pandemic requirements. There are some recommendations that can help these systems prepare for future pandemic occurrences, such as:
- Return air tracking boxes paired with a supply box to allow room control of pressurization. This will allow an easier modification to negative pressure for the standard patient rooms.
- Pandemic exhaust fans dedicated to floors or wings by utilizing return air pathways to each floor. This will allow floors to be converted to negative isolation floors (see Diagram 1).
- Cooling coils will be sized to handle 100% outdoor air at peak loads. This will allow the AHUs to operate in 100% outside air mode year-round.
- Designing an exhaust purge mode that is able to flush the hospital floor by floor. The system will need to have the ability to activate an exhaust fan that is only activated during the purge mode.

DIAGRAM 1. An air-handling unit control diagram.
CONCLUSION
Ventilation systems on their own are not the end-all, be-all engineering solution to minimize the airborne transmission of viruses like COVID-19.
Ventilation systems are most helpful when combined with other hospital airflow systems, such as HEPA air filtration, ultraviolet germicidal irradiation (UVGI), and other means of deactivating viruses, bacteria, and other microorganisms. Efficacy of the HEPA filtration and UVGI on the COVID-19 virus is still under investigation, but based on their effects on other viruses, it can be inferred that they will impact the virus’s activity in an airflow system. Care must be taken to ensure the modification of one part of a ventilation system does not negatively affect the overall air system’s performance. One thing that is certain is that designers cannot design ventilation systems without at least considering future pandemic occurrences.