Several years ago, I was contracted to perform an evaluation study for an existing biosafety level-3 (BSL-3) biocontainment laboratory on the West Coast. The lab was actively performing research on anthrax, tuberculosis, and other aerosolized pathogens. The facilities were 10 years old, and the client wanted the study to compare an existing lab facility assessment versus the latest National Institute of Health (NIH) Biosafety in Microbiological and Biomedical Laboratories standards as well as an evaluation of the existing facility condition with recommended repairs/replacement.
This article will provide an explanation on the biocontainment laboratory classifications levels, types of biosafety cabinets (BSCs) used in BSL-3 labs, NIH requirements for a BSL-3 lab, description of the BSL-3 lab being assessed, recommended procedures for performing a BSL-3 lab assessment, and what was discovered during the BSL-3 study. Though the study was comprehensive in evaluating the overall lab layout, architecture, security, electrical, HVAC, and plumbing; this article will focus on the HVAC systems.

Biocontainment Laboratory Classification Levels
Excluding animal biocontainment laboratories, biocontainment laboratories are classified as one of four levels. The more virulent and infectious the pathogen being worked on in the laboratory, the higher the classification level will be for the lab. It is important to know BSC are considered the primary barrier for containing the pathogen. The lab space and associated facility systems are considered the secondary barrier for containing the pathogen. The four levels have a hierarchy with all practices and procedures established on the lower level being carried over to the higher level. Descriptions of the four biosafety levels as follows:
- Biosafety Level 1 (BSL-1) — This is the most basic biosafety level. Typically, personnel work with low-risk, well-characterized pathogens that pose little to no risk of infection in healthy adults. Infections are not life-threatening. There are affective medicines for treating the infected. BSL-1 laboratories do not require a primary or secondary barrier, separation from general traffic patterns, access control beyond a door, negative space differential pressure, a dedicated HVAC system, or a dedicated exhaust system.
- Biosafety Level 2 (BSL-2) — This biosafety level has personnel working with pathogens that are known to cause human disease and pose a moderate risk to personnel and environment. Infections are transmitted through the skin, mucous membrane, or ingestion exposure, not via aerosol. Infections can cause severe disease or death. There may be partially affective medicines for those infected. BSL-2 laboratories may have primary and secondary barriers, separation from general traffic patterns, access control, negative space differential pressurization, lab material decontamination, and a dedicated HVAC and exhaust system. The primary barrier can be a Class 1 or Class 2 BSC.
- Biosafety Level 3 (BSL-3) — This biosafety level has personnel working with pathogens that are known to cause human disease and pose a serious risk to personnel and environment. Beyond the paths of transmission noted for BSL-2, there is a substantial risk of becoming infected through the inhalation route. For example, COVID-19, tuberculosis, and anthrax are BSL-3 level microbes. Infections can cause severe disease or death. There may be partially affective medicines for those infected. BSL-3 laboratories have a higher emphasis on primary and secondary barriers with all laboratory manipulation being performed within a BSC. The lab spaces are separated from general areas by anterooms or airlocks. Autoclaves and liquid waste kill systems are used. The lab shall have negative space differential pressurization with air flowing from uncontaminated spaces to contaminated spaces. The lab shall be provided with a dedicated once-through HVAC system and exhaust system with HEPA filters. The lab and associated HVAC and exhaust system must be designed for decontamination. Depending on the required parameters, for Class 2 – types A1, A2, B1, and B2, BSC are used. Typically, Class 2A2 and 2B2 are the most commonly used BSC in BSL-3 labs.
- Biosafety Level 4 (BSL-4) — This biosafety level has personnel working with the most dangerous and exotic pathogens that pose a high risk of aerosol-transmitted infections. BSL-4 microbes cause life-threatening diseases that are frequently fatal for which there are currently no vaccines or treatment. Ebola and hemorrhagic viruses are BSL-4 pathogens. BSL-4 lab requirements are more complex than those for BSL-3 lab. Exhaust systems require double-HEPA filtration. The HVAC and exhaust system need to provide a higher level of reliability. Typically, Class III BSC are used.
BSL-4 lab requirements are more complex than those for BSL-3 labs. Exhaust systems require double-HEPA filtration. The HVAC and exhaust system need to provide a higher level of reliability. Typically, Class III BSC are used.

Different Types of BSCs
There are three different classes of BSCs: Class I, Class II, and Class III. Within Class II, there are four types, including A1, A2, B1, and B2. In selecting a BSC, it is important to determine whether the unit is providing protection for the personnel and surrounding environment and/or protection of the pathogen being worked on. Class I BSCs protect personnel and the environment but not the pathogen being worked on. Class II BSCs protect personnel, environment, and the pathogen being worked on. Class III, which is known as glove boxes, provides a physical barrier between personnel and the pathogen. For BSL-3 laboratories, Class II, type A2 and B2 BSCs are primarily used.
- BSC Class II Type A2 — Looking at Figure 1, the BSC has an internal blower, which draws room air in through the front grille of the cabinet. The contaminated air is then pushed into the central plenum, where approximately 30% of the contaminated air is exhausted out of the cabinet through a HEPA filter, and the remaining 70% is recirculated back into the cabinet work zone through another HEPA filter. The recirculation airflow is unidirectional (laminar). The exhausted airflow can be recirculated into the room or exhausted through an indirect canopy connection. Class II A2 safety cabinets are used where there are minute quantities of hazardous chemicals.
- BSC Class II Type B2 — Looking at Figure 2, the BSC has an internal supply air blower that draws in room air and supplies to the cabinet work zone through a HEPA filter. The BSC has direct exhaust connections that exhaust the supply air and room through the sash. The exhaust needs to maintain a minimum 100 feet per minute (fpm) through the cabinet sash opening. Class II B2 safety cabinets are used where hazardous chemicals or radio isotopes are used.
Recommended Procedure for Performing a Site Assessment
Performing a BSL-3 site assessment should include preplanning the site observations, performing the site observations, interviewing laboratory and maintenance personnel, and performing HVAC system and BSC testing.
- Preplanning Site Observations — Performing site observations and testing at a high-containment biological laboratory takes substantial planning. Planning considerations include familiarizing yourself with a final record set of drawings and controls before the site observations, working during evenings or weekends to reduce the disruption to laboratory operations, removing microbes and decontamination of the laboratory; scheduling personnel/contractors that maintain the facility and control systems to attend walk throughs, scheduling a test and balance (TAB) contractor; and scheduling laboratory personnel interviews. Depending upon laboratory operations, scheduling the site observations may take several months to coordinate.
- Site Observations — Site observations need to be thorough and well-planned. As a minimum, the entire HVAC and exhaust system needs to be inspected. Does the installed mechanical system and controls match the furnished construction documentation? What is the physical condition of the equipment, equipment components, and ductwork distribution system? Were the equipment and ductwork installed properly, and is the equipment accessible for maintenance? Are there any observable construction defects? Are the mechanical system controls active and functioning?
- Interviewing Laboratory and Maintenance Staff — Laboratory staff should be interviewed on what procedures they are performing in the laboratory and how those procedures integrate with laboratory facilities. What is the decontamination procedure? Are there any specific concerns the staff has in regard to the laboratory facility or its operation? Maintenance staff should be interviewed on the mechanical system operation and any possible issues. Any available mechanical system logging data and sequence of operations should be obtained. And, the following questions should be anwered: What is the maintenance program for the HVAC system? How often is the HVAC system tested and balanced? How often are sensors and controls calibrated?
- HVAC System and BSC Testing — BSCs are the primary barriers for protecting personnel while working with pathogens. The National Science Foundation established NSF/ANSI Standard 49 for the design, construction, performance, and field certification of Class II BSCs. There is an extensive list of testing procedures that needs to be performed to certify as a Class II BSC. For the Class IIB2 BSCs being evaluated, the cabinets were previously tested for pressure decay, drain spillage trough leakage, and airflow stability. The lab personnel noted there were no high-noise complaints, and the noise level testing was not performed. The biosafety test was focused on the overall airflow performance, and testing included HEPA filter leak testing, vibration testing, down-flow velocity testing, in-flow velocity testing, airflow smoke patterns testing, and motor/blower performance. The dedicated HVAC system and exhaust system testing and balancing should include air-handling unit (AHU) supply air temperature, supply air duct pressure, supply venturi valve airflow, supply air venturi valve static pressure drop, exhaust air venturi valve airflow, exhaust air venturi valve static pressure drop, exhaust HEPA filter static pressure drop, exhaust fan airflow, exhaust ductwork static pressure, space pressurization relationships, space temperatures, space humidities, AHU fan and coil performances, and exhaust fan performances. Testing is performed for each mode of operation.

National Institute of Health (NIH) Requirements for a BSL-3 Lab
Some of the NIH HVAC requirements for a BSL-3 lab include:
- A dedicated HVAC system that does not serve other portions of the building.
- The HVAC system and exhaust system have N+1 equipment redundancy and should be designed to operate at all times.
- Lab space environmental conditions to be 73ºF +/- 2º and 50% +/- 5% RH during summer and 70º +/- 2º and 30% +/- 5% RH during winter.
- A minimum ventilation rate of 6 AC/HR.
- HVAC and exhaust systems create a once-through airflow.
- Space pressurization cascade is from lower-hazard spaces to higher-hazard spaces. The pressurization cascade is established by having 100 cfm traversing around doors.
- Supply air and exhaust air shall be ducted. No return air plenums are allowed.
- The AHU is to be provided with a MERV-8 pre-filter and MERV-14 final filter. The exhaust system shall be provided with HEPA filters in a bag-in/bag-out housing.
- The HVAC and exhaust systems shall be placed on emergency power.
Description of the BSL-3 Lab Being Assessed
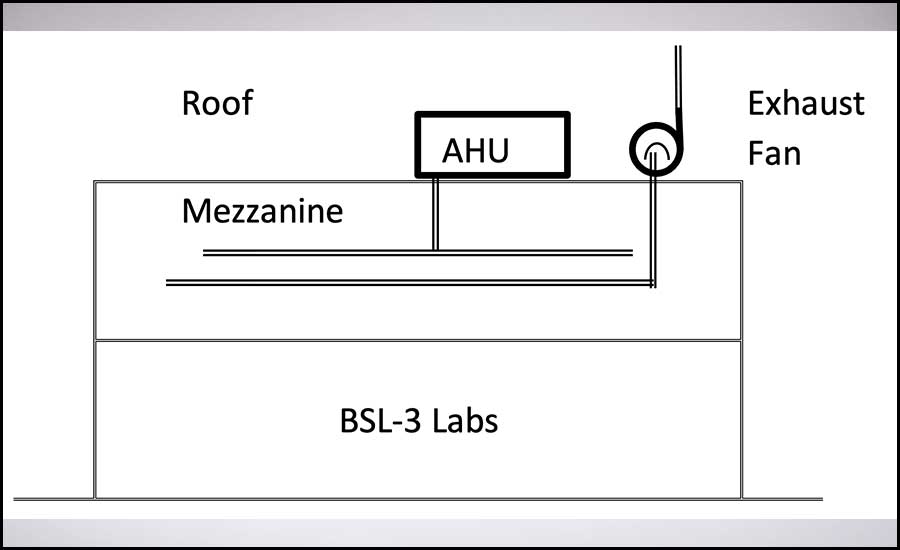
The BSL-3 laboratory is located in a large, single-story building that contains general chemistry labs, office space, mechanical spaces, and electrical spaces. The lab layout consists of ante room, gowning rooms, a clean corridor, lab spaces, BSC spaces, a decontamination space, and autoclaves (see Figure 3). There is a dedicated mezzanine above the lab for accessing the ductwork, control valves, and exhaust system HEPA filter bank (see Figure 4). The lab has dedicated HVAC and exhaust systems that were located on the roof next to each other (see Figure 4). The chilled water system and heating water system were located in a dedicated mechanical room.
The lab space pressurization had the ante-room with the lowest negative space pressure with the space pressure reducing through the gowning to the clean corridor, lab spaces, and finally with the BSC spaces having the most negative space pressurization (see Figure 5).
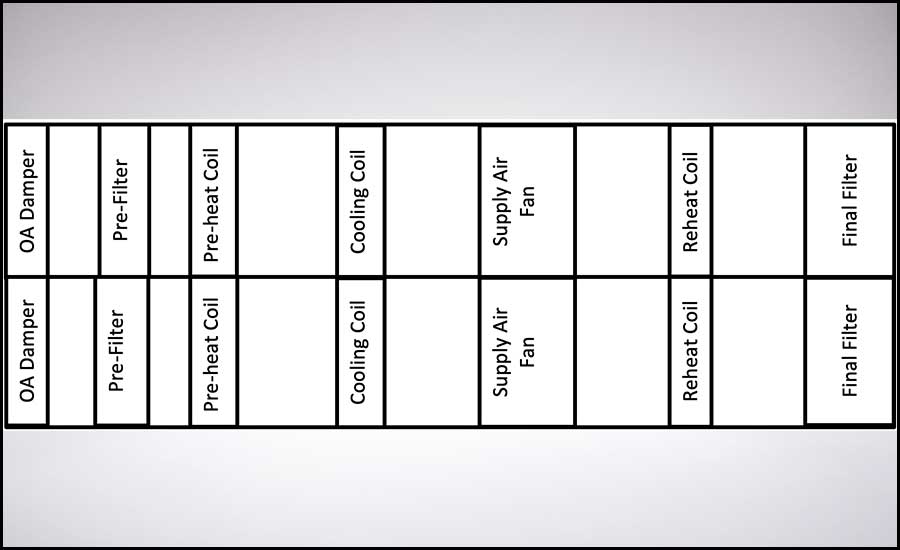
The AHU has two tunnels with either of the tunnels able to meet the lab supply airflow, cooling, and heating requirements. The AHU has a MERV-8 pre-filter and MERV-14 final filter (see Figure 6). The exhaust system has dual-exhaust fans bypass air plenum (see Figure 7).
The space temperature readings ranged between 71º-74º, and the relative humidity (RH) ranged between 47%-53%.
The HVAC control philosophy has the AHU and exhaust fan on the building management system (BMS) while the supply air and exhaust air venturi valves were on a separate control system. The basic supply air control philosophy was to maintain 2 inches of water gauge (INWG) supply duct pressure during occupied modes and 1 INWG during unoccupied modes. The supply air and return air venturi valves are designed to modulate to a lower airflow set point during unoccupied mode.

BSL-3 Study Findings
The BSL-3 lab evaluation found many things that were good, bad, and ugly. The good are items that meet the industry standard of care, the bad are those that have the potential to cause substantial contamination, and the ugly are items that have a high probability of causing unwanted contamination.
The Good
- The once-through HVAC system met NIH requirements.
- The HVAC system was in good condition.
- A maintenance floor was provided above the laboratory for easy maintenance access to supply air valves, exhaust air valves, and mechanical equipment.
- The lab space air change rate met NIH requirements.
- Space temperatures and RH met NIH requirements.
- Space-to-space pressurization cascade went from the least contaminated space to the most contaminated space.
- Space supply air diffusers did not impact BSC inlet air profile.
- BSC operation met NSF 49 requirements.
- The chilled and heating water plants met N+1 equipment requirement.
The Bad
- Main exhaust fan bearings are severely damaged and ready to fail. Both exhaust fans were operational.
- The building’s fire alarm system, which predominantly serves nonclassified spaces, shuts down the BSL-3 laboratory HVAC and exhaust systems when tripped.
- There was a failed space differential pressure sensor to the most negative lab space. The temperature, RH, airflow, and space differential pressure sensors have not been calibrated since their initial installation.
- Maintenance staff did not understand how the BSL-3 laboratory really operated.
- There are no space smoke detectors in the lab spaces.
The Ugly
- The supply air venturi valve serving the decontamination space was installed backwards during the original installation and had not worked in 10 years of operation.
- The supply air and exhaust air venturi valves' controls were not interconnected to the HVAC system control system. These valves have not modulated in 10 years of operation. When the HVAC system went into unoccupied mode of operation, which consisted of reducing the AHU discharge static pressure, the static pressure across the supply air valves was below the manufacturer’s minimum requirement. Remarkably, with the supply air valves in their fully open position, the required space pressurization relationships were maintained.
Recommended Repair/Replacement
Based upon the site observations, testing, and analysis, the following changes are recommended:
- Remove and properly install the improperly installed supply air venturi valve.
- Replace supply air and exhaust air fan bearings.
- Rebalance fan squirrel cages.
- Refurbish humidifier.
- Replace the AHU inlet damper and actuator.
- Recalibrate all control sensors to National Institute of Standards and Technology (NIST) standards.
- Replace chilled water and heating water control valves and re-insulate the associated piping above the roof.
- Modify the exhaust fan discharge cone to maintain 3,000 fpm minimum discharge velocity and perform computational fluid dynamics (CFD) modeling of the exhaust plume.
- Order spare AHU chilled water and heating water coils.
- Empirically test supply air and exhaust air duct static pressure set points. Reduce the static pressure set point to where the minimum venturi air valve static pressure drop is 1 INWG.
- Revise AHU and exhaust fan control systems and sequence of operation to be fully integrated.
- Require the BSL-3 space smoke detector to trip before HVAC and exhaust systems are shutdown.
Conclusion
The lab owner had the foresight to have the laboratory assessed after 10 years of operation. Though the laboratory had no prior contamination issues and the HVAC system operated adequately enough to provide reasonable environmental conditions, the HVAC and exhaust systems needed substantial repairs and renovations to meet the original system design intent and ensure reliable future operation.
References
- National Institute of Health Biosafety in Microbiological and Biomedical Laboratories, 6th Edition, Revised June 2020.
- National Institute of Health Design Requirements Manual, Revision 1.5, 3/5/2020.
- Phoenix Controls Corporation BSL-3 Laboratory Design Resource.
Vincent Sakraida is a mechanical engineer lead at PCI Salas O'Brien. He boasts more than 35 years of experience in the design, construction, and operation of cleanroom, pharmaceutical, laboratory, and other high-technology facilities. He is also a member of the ASHRAE Epidemic Task Force Laboratory Subcommittee. Contact him at bsme82@comcast.net.