Throughout human history, “good buildings” have been defined by measurable benchmarks tied to creating wealth.
Millions of years ago, shelters were seen as tools that enabled vulnerable humans to survive. Building performance metrics were likely determined by a community’s population.
As populations switched from hunter-gatherer to agrarian lifestyles, surviving dwellings from the Stone Age revealed their role in the preservation of food and supplies. Again, the success of these buildings was probably based on the number of people that the accumulated materials and food could support.
By the Industrial Revolution, building uses expanded to support manufacturing and the workers needed to run machines. The value of these buildings was directly linked to wealth from industry and disconnected from natural processes, such as farming.
The definition of a high-performing building evolved again following the oil embargo of the 1970s. New rating systems emerged during this “green building” movement to standardize reduced carbon-based fuel consumption during construction and ongoing building operations.
Throughout time, the ease in measuring building success has remained. Changes in food storage, bank account balances, and energy meters are easy to quantify and track.
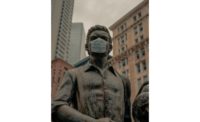
Now, we are dealing with a more challenging metric. In March, as COVID-19 took hold and spread, people rapidly vacated office buildings, gyms, stores, and other public buildings. Coming full circle, the oldest and most important building function is once again in sharp relief. Buildings are medicine. More compelling than human productivity, cognitive functioning, and comfort, buildings must shelter us from infectious diseases — or at least not serve as reservoirs of contamination.
Building owners are now struggling to achieve safe building conditions and communicate this to draw tenants and occupants back.
Toward this end, many rating systems and certifications have arisen or expanded to align building management with greater visibility of IAQ testing and HVAC operations, which are seen as key to giving people confidence to reoccupy buildings. The trouble is, before we can operate truly protective indoor environments, we must identify, measure, and manage health-related metrics. Unfortunately, verifying indoor standards created for reducing energy use will not preserve human health.
Standards and certifications, such as WELL, Fitwel, LEED, British Standards Institute (BSI) guidelines, RESET, and the Building4Health (B4H) Canary platform, are gaining traction in high-end commercial buildings. These differ in the components monitored for certification.
Despite the clear need to collect data on the effect of IAQ on infection risk and occupant health, there are several obstacles. One hurdle is possible apprehension that the mere existence of data, even when collected with the good intention of improving building safety, could create a legal risk. If an occupant or employee gets sick, initiates a lawsuit, and the records are subpoenaed, what might happen? A second obstacle is the difficulty in creating a direct cause-and-effect link between indoor exposures and health or disease. Unlike the clear connection between building characteristics and injuries from fires or earthquakes, IAQ-related health changes are often delayed, introducing the possibility of effects from non-building exposures.
Despite these challenges, COVID-19 has revealed the economic consequences of empty buildings. For this to change, we must give people confidence to occupy buildings by creating and following medically based health standards for IAQ.
Here is a list of five things you can do: Realize that the health of building occupants, both now and after COVID-19, is strongly affected by indoor air management; refresh your understanding of microbiology and human physiology; work with ASHRAE to include health outcomes in building standards; encourage building owners to realize the cost benefits of healthy human occupants by developing and sharing your own business models; and when you see your own primary care provider, educate them about the importance of IAQ in disease prevention.