According to the United Nations, primary health care can meet 90% of a community’s needs. Primary care — medical care that focuses on health and well-being, including preventive health, such as vaccinations and education — is a vital part of the health care continuum. It proactively and efficiently addresses the main causes of illness and poor health. Regular primary care reinforces healthy activities, prevents and reduces disease incidence, identifies and manages developing or chronic illnesses, and guides patients through the medical system, should they need specialty care. Yet, nearly 50% of insured adults skip their primary care. In addition to costs, patients' reasons for missing routine care include being too busy, the inconvenience, appointment delays, the clinic is too far away, or lack of transportation. The rate of the uninsured or underinsured who forego primary care is even higher. This overall health care deficit costs the U.S. an estimated $67 billion every year.
Despite the importance of primary care, not everyone in the U.S. has access to a provider. In 2017, about 30% of men and 17% of women in the U.S. did not have a primary care provider. The percentages are higher among underserved communities and in certain parts of the country, such as Nevada, Texas, and Alaska. Instead, these people try to manage at home and use urgent care clinics and emergency rooms when they need care.
Bring Primary Health Care to the Patient
What if the 8,000 miles of commuter and passenger rail in the U.S. could be used to bring primary care to patients across the country, from urban centers to the rural countryside? The concept, called Fare2Care (F2C), uses specially outfitted medical cars coupled to regular commuter trains, bringing health care access to hundreds of stations across the country.
The F2C cars work with existing mass transit and rail systems, including those that reach underserved communities. They can also be adapted to different rails systems when and where needed. Care cars can be converted to road-capable dual-mode vehicles (DMVs), rotating through underserved communities, bringing these clinics to remote, “last-mile” service points that lack primary care access.
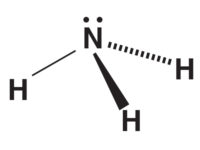
Each F2C car includes up to four exam modules, where a patient can communicate with his or her doctor or other care provider(s) through an interactive screen and mobile telecommunication system. Automated sensor technology provides health screening and basic diagnostics, while integrated robotics perform blood draws and injections and dispense common medications. If it is determined that patients require an in-person visit, the doctor or nurse can make arrangements or transport the patient directly in urgent situations.
When each patient leaves, the car is cleaned with robotic cleaners that use UV-C and far-UV lights to disinfect and limit contamination risk. In-duct UV-C lights decontaminate room air while bipolar ionization in each station's HVAC system further limits the transfer of air contaminates on the station platforms. In addition, the cars are kept at a relative humidity between 40%-60% (when possible) to reduce viral spread.
The cars can also be adapted for other uses. Larger modules can fit a group of people who gather for a therapy session, for example. Cars can also be outfitted and deployed in cases of mass testing, vaccinations, or injuries.
Technology Keeps System Secure
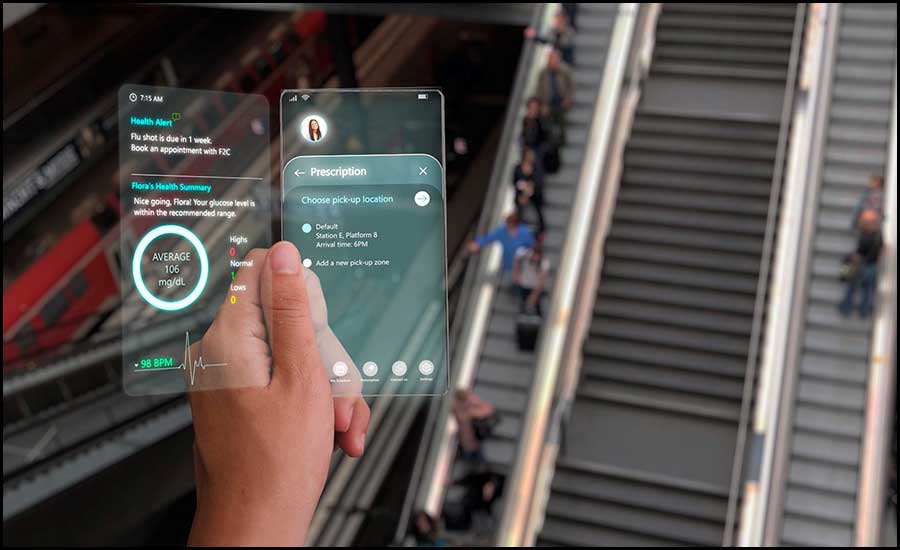
F2C's secure technology connects users with car services using a smartphone app or smart tickets for one-time users or those without mobile phones.
The dedicated app, e-ticket, or printed smart ticket is used to make appointments and provide information. Patients can keep track of their health records, schedule appointments, refill medications, communicate directly with their doctors, and check train schedules.
The app or ticket controls access to the care module through a dedicated, secured hallway. After reaching the care module, admission is only possible if the patient has a valid appointment. Each scan is unique to each user to maintain patient privacy and security. No one else can gain access.
Technology Identifies Users Who Should See a Doctor
When users enter an F2C participating station, an early detection system, similar to Amazon Go’s technology, detects elevated body temperatures. If commuters are identified as having an elevated body temperature, they are directed to an F2C car for assessment. If the system suspects an infectious disease, the care car decouples at the next stop, rerouting to the closest hospital.
F2C can provide services to a wide range of patients, from those who need help for a one-time issue to continuing chronic care. Easy access to F2C can be an advantage for those managing chronic illnesses, ensuring the patient receives consistent treatment. For example, people with diabetes need to monitor their blood sugar levels and take varying insulin doses. Regular appointments in an F2C car, to and from work or school, ensure consistent blood tests and correct insulin doses. Close monitoring also reduces the risk of diabetes complications.
People with limited mobility — either using a wheelchair or a walking aid — may find it challenging to travel long distances or access some offices or clinics. Whether they need regular checkups for blood tests or other health issues or want to see a doctor about a new problem, F2C cars are accessible for their primary care needs.
Follow-up appointments are also available for people monitoring recovery from a prior illness or procedure.
Potential Partnerships
For F2C to succeed, it must partner with municipalities to bring together its local transportation and health systems to reach target populations. Improved population health through broadened access to primary care can positively impact local economies. City leaders could also leverage F2C in times of public health crises, such as mass testing or immunization, keeping more citizens healthy.
The average commute on public transit varies depending on the city or town, but many major urban areas have an average commute time of one hour in each direction. By using F2C, users do not have to take time off work, reducing their productivity or increasing costs to their employers if they need to use replacement workers. Trips to the doctor will also no longer infringe on personal or family time.
Through F2C, SmithGroup is creating an entirely new primary care ecosystem deployed through America's existing public transit infrastructure. By adding F2C cars to existing rail systems, patients can get care while commuting, shortening waiting time, increasing accessibility, and expanding preventive care while simultaneously de-stressing the health care system, reducing health care costs, and improving individual and population health.
Download to learn how Fare2Care delivers accessible primary care.
SmithGroup's F2C design solution was selected as a finalist for the 2020 Healthcare Design Breaking Through competition. The competition encourages innovation by asking participants to solve challenges in the future delivery of health care without the usual restrictions tied to budget, schedule, and codes. The SmithGroup team developed a novel concept that provides more convenient and equitable primary care access by leveraging existing transportation infrastructure. The concept is forward-facing but could be implemented within just a few years, given predicted advances in virtual technology.