People are the reason excellent health care design matters — whether they are working or seeking care.
“When a flower doesn’t bloom, you fix the environment in which it grows, not the flower.” This quote, and others similar to it, have been used over the years to highlight how important an environment is in promoting personal well-being. The quote can be applied to child and adult development, relationships, parenting, work environments, and, certainly, the health care built environment. It is a very powerful idea. The decisions we make as engineers during design should always echo this idea and, as daunting a task as it may seem, walking the path of designing exceptional environments is well within reach.
Even though health care is ever changing, there are many engineering and design tools that provide guidance and help establish a minimum baseline to achieve health care environments that support growth, healing, and happiness for not only patients but all health care workers, administrative staff, and visitors who work in and visit these facilities.
"When a flower doesn’t bloom, you fix the environment in which it grows, not the flower." Quote courtesy of Alexander Den Heije
In addition to utilizing codes, standards, and guidelines to provide guidance, MEP design engineers are often called upon to provide recommendations for best practice. These recommendation’s cover everything from possible system approaches; parameters for defining required loads; equipment capacities; and methods of redundancy to space layout, equipment locations, routing, and future flexibility.
However, the needs/requirements for a health care building to promote healing is an essential part of the functionality of each building, whether it be a Level 1 trauma center, a surgery center, outpatient clinic, or standard inpatient hospital. Determining how the mechanical systems integrate into buildings become an important part in creating a positive and healthy work environment. Furthermore, the marrying of code-required design with engineering best practices is essential to reaching that goal but can become tricky and problematic when trying to determine which systems can provide those aforementioned ‘staples of engineering design’ versus the cost associated with them and agreeable returns on investments (ROI).
This article will provide general guidance for all mechanical engineers designing health care facilities; help bridge the gap between the code requirements and engineering best practices necessary to support a healthy building environment; and look at how designs could change or adapt in response to real-life conditions, code changes, and client demands, especially today, in light of our current pandemic challenges and the very real risk of recurrences in the future.
Understanding the ‘Codes’ and Best Practices
There are a number of codes and standards that come into play when designing health care facilities, but the two major ones utilized in almost all municipalities and, to some degree, across the world are referred to as the Facility Guidelines Institute (FGI) Guidelines and ASHRAE Standard 170.
The FGI is a nonprofit organization that works to develop guidelines for designing and building hospitals and other health care facilities. These guidelines have been adopted in some form by municipalities across the U.S./world and inform on everything from room requirements, room sizes, and room quantities to the number of restrooms, sinks, or emergency power receptacles.
ANSI/ASHRAE/ASHE Standard 170 took root in 1999, when ASHRAE determined that an American National Standards Institute (ANSI)-approved standard on ventilation in health care facilities was needed. This standard was continually developed over the years and formally became ANSI/ASHRAE/ASHE Standard 170 in 2008. The FGI guidelines and ASHRAE 170 carried some duplicate information for many years, but, in 2018 the FGI Guidelines formally removed repetitive language and tables and referred the user to ASHRAE Standard 170 for mechanical and ventilation requirements in health care facilities. Municipalities that have adopted the FGI guidelines as code have, in turn, adopted ASHRAE Standard 170 as code.
 FIGURE 1: An excerpt from ANSI/ASHRAE/ASHE Standard 170-2017 showing part of Table 7.1 that defines pressure relationships, room air exchange rates, and temperature/humidity ranges, among other things.
FIGURE 1: An excerpt from ANSI/ASHRAE/ASHE Standard 170-2017 showing part of Table 7.1 that defines pressure relationships, room air exchange rates, and temperature/humidity ranges, among other things.
ANSI/ASHRAE/ASHE Standard 170 defines ventilation system design requirements that provide environmental control for comfort, asepsis, and odor in health care facilities. To accomplish these objectives, the standard provides guidance on space air change rates, ventilation rates, environmental conditions, pressure relationships, redundancy, and more (see Figure 1).
In engineering design, best practice is most easily defined as designing above and beyond the code minimum to augment the system concepts while providing value and reasonable thought. For example, Standard 170 calls for two low air return grilles to be placed at opposite corners in an operating room, but four low air return grilles, one in each corner, is considerably better for capturing of particles in a room and removing them. Design recommendations like this move beyond the realm of bare minimum design solutions and begin to enhance the quality of environments that are more conducive to healing and overall well-being for patients, health care workers, and visitors.
As Table 7.1 (Figure 1) illustrates, mechanical engineers designing health care facilities should also be aware of the importance of properly controlled humidity within a space. It has been proven that the standard’s listed relative humidity range (as illustrated in the ‘Sterling Chart’ – Figure 2) will create healthier buildings for occupants by reducing the risk of pathogenic infection while optimizing immune defense mechanisms.
 FIGURE 2 The Sterling Chart – 2016 ASHRAE Handbook – HVAC System and Equipment, Chapter 22, indicates ranges of relative humidity and optimal zones for production or grow of negative environmental components.
FIGURE 2 The Sterling Chart – 2016 ASHRAE Handbook – HVAC System and Equipment, Chapter 22, indicates ranges of relative humidity and optimal zones for production or grow of negative environmental components.
Mechanical Design for Critical Spaces
Since environment plays such a vital role in promoting faster recovery times, happiness, and well-being, let us focus on a few areas within hospital environments where proper design is most critical. The section below highlights code minimums and then provides design considerations that go above and beyond the bare minimums.
CENTRAL STERILE PROCESSING DEPARTMENT
The central sterile processing department (CSPD or SPD) is the area within the hospital that provides a centralized service for instrument processing, decontamination (coupled with cart washer), sterilization, case part preparation, and storage. Typical room names in this service line are decontamination, sterile processing, and sterile storage.
• Code - ANSI/ASHRAE/ASHE 170:
o Decontamination: 6 AC/HR / negative pressure (@ minus 0.01 inches water gauge [INWG]) / 100% exhaust / 63°-70°F.
o Sterile processing and sterile storage: 4 AC/HR / positive pressure / 68°-73°F.
• Design Considerations:
o Exhaust air diffusers should be located at/above sterile processing equipment or heat-generating equipment and inboard to the room. Supply air diffusers should be located on the opposite end of the room so as to cause airflow to move from clean to less clean. Exhaust air should be constant; supply air should be modulated to maintain a minimum minus 0.015 INWG. Due to the amount of air that may be required, supply linear diffusers may be a good option, located at the opposite end of the room from the exhaust locations.
o Differential Static Pressure Sensors (DPS) should be located at each door into decontamination and at the entrances to the sterile rooms. Pressure should be averaged between sensors for each room and controlled by averaging differential pressure to the respective room supply air.
o A dedicated exhaust air fan allows for better control and balancing of the spaces within.
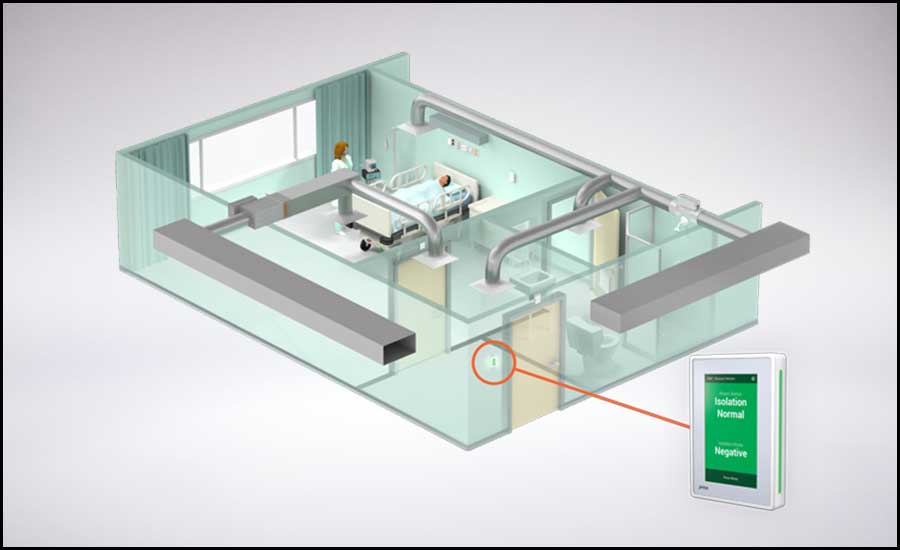 FIGURE 3: Combination airborne infection isolation/protective environment (AII/PE) rooms showing layout and the location of the differential static pressure sensor (DPS). Photo courtesy of Antec Controls
FIGURE 3: Combination airborne infection isolation/protective environment (AII/PE) rooms showing layout and the location of the differential static pressure sensor (DPS). Photo courtesy of Antec Controls
OPERATING ROOMS
• Code - ANSI/ASHRAE/ASHE 170:
o Four AC/HR outdoor air / 20 AC/HR total / positive pressure / 68°-75°F / 30%-60% humidity.
o Two low air returns at opposite corners of the room.
o Positive pressure @ +0.01 INWG.
o Coverage of the primary supply diffuser array shall extend a minimum of 12 inches beyond the surgical table and the diffuser array shall cover a minimum of 70% of this area.
• Design considerations:
o Engineers must be aware of the surgeon’s requirements for the OR’s they are designing. An operating room needing 65°F @50% RH needs a 43°F supply air temperature off a cooling coil to allow for 50% RH in the space. Desiccant dehumidification may be necessary.
o Design for positive pressure of +0.015 INWG. Designing at +0.015 INWG provides more positive air movement from clean to less clean and helps to avoid nuisance alarms and sensor tolerances as well as door openings and closures.
o Provide four low air returns in each corner of the room. CFD modeling has shown this is a more effective strategy when pulling air down and away from the patient.
o Provide 23-25 air changes an hour total. This allows for testing and balancing tolerance as well as leakage in the space.
o Provide 100% primary supply diffuser array over the surgical table in lieu of 70%. Coordinate boom locations and lights to be outside the primary supply array.
COMBINATION AIRBORNE INFECTION ISOLATION/PROTECTIVE ENVIRONMENT (AII/PE) ROOMS (FIGURE 3)
• Code - ANSI/ASHRAE/ASHE 170:
o Two AC/HR outdoor air / 12 AC/HR total / positive pressure / 100% exhaust / 70°-75°F / 60% max humidity.
o Supply diffusers above the patient bed and exhaust diffusers located near patient room door.
o Positive pressure @ +0.01 INWG.
o HEPA-filtered air.
o Provide Group E, nonaspirating supply diffusers, i.e., laminar flow diffusers.
• Design considerations:
o Design for positive pressure of +0.015 INWG. Designing at +0.015 INWG provides more positive air movement from clean to less clean and helps to avoid nuisance alarms, and sensor tolerances address loss from door openings and closures.
o Provide 14 AC/HR total. This allows for testing and balancing tolerance as well as leakage in the space.
o Provide no supply air (SA) in the typical AII patient room toilet area and allow the exhaust from this space to contribute to the negative pressure requirement while providing better air diffusion throughout the rooms.
o If the design calls for a large quantity of these rooms, provide an independent air-handling unit with HEPA filtration to serve these spaces only
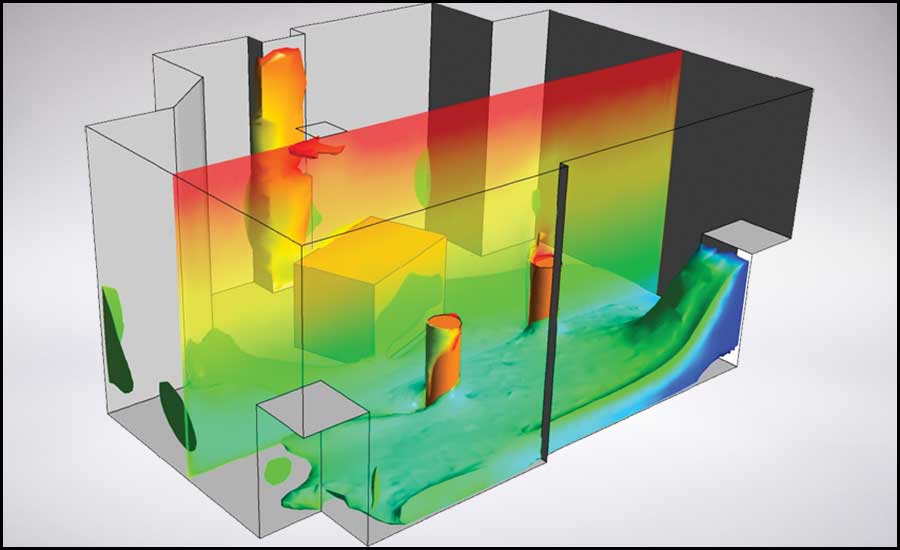 FIGURE 4: Thermally stratified environments – showing cool air at the floor with warmer air above the occupied zone.
FIGURE 4: Thermally stratified environments – showing cool air at the floor with warmer air above the occupied zone.AII ROOMS
• Code - ANSI/ASHRAE/ASHE 170:
o Two AC/HR outdoor air / 12 AC/HR total / negative pressure / 100% exhaust / 70°-75°F / 60% max humidity.
o Exhaust diffusers above the patient bed or on wall at head of bed.
o Negative pressure @ minus 0.01 INWG.
• Design considerations:
o Design for negative pressure of minus 0.015 INWG. Designing at minus 0.015 INWG provides more negative air movement from clean to less clean and helps to avoid nuisance alarms and sensor tolerances as well as door openings and closures.
o Provide 14 AC/HR total. This allows for testing and balancing tolerance as well as leakage in the space.
o Provide no SA in the typical AII patient room toilet area and allow the exhaust from this space to contribute to the negative pressure requirement while providing better air diffusion throughout the rooms.
Other Considerations to Providing a Better Building Environment
Room pressure control, addressed in Paragraph 6.7.1 of ANSI/ASHRAE/ASHE Standard 170, states: “Maintain the pressure relationships required in Tables 7.1, 8.1, and 9.1 in all modes of HVAC system operation…” Designing to and maintaining pressure differentials between zones will evoke tighter environmental control by influencing the directional flow of air from clean to less clean environments. Outside of Brownian motion, airflow is the cause of particle motion, so controlling pressure is an effective means of controlling the directional paths of airflow from one room to the next. The application of this strategy is vital to maintaining clean healthy air in critical care areas such as AII, protective environments (PE), and operating rooms. Controlling these PE spaces and ORs to a positive pressure reduces the risk of immunocompromised patients or those with open wounds during surgery from becoming infected by airborne germicides. To validate the assigned pressures are maintained, the standard states that specific critical care areas, such as AII rooms, “…shall have a permanently installed device and/or mechanism to constantly monitor the differential air pressure between the room (when occupied by patients) with a suspected airborne infectious disease and the corridor....”
Alternative System Design Considerations (Thinking Beyond Variable Air Volume Systems)
Health care environments can be affected at the room level or building-wide. Let us explore three building system strategies that, when properly applied, will expand the design intent of promoting healing and the overall well-being of occupants. Each of the items mentioned in the next section are designed to optimize IAQ, leading to the reduction of pathogens, the recirculation of air throughout a building, and the movement of air from clean to less clean.
Displacement Air Systems
Unlike a mixed air system that injects ~55°F air overhead into a space at high velocity, displacement ventilation supplies warmer air into a space at low velocity through diffusers with large face areas mounted low in the wall creating a thermally stratified environment. Using the principles of convection, thermal stratification uses heat sources in a space to move the air. Any heat source with a surface temperature greater than 75°F will create a thermal plume that will continually rise to the upper levels of a room. Unlike VAV mixed air systems that may be subjected to airflow changes depending on room load, displacement ventilation will allow for a continual stream of air from the occupant zone to the upper levels of a room where the return and exhaust air grilles are located, allowing for contaminated air to be more readily removed from a space. Displacement systems are more forgiving in how air behaves in a space depending on geometry and occupant locations. A thermally stratified room (see Figure 4) will tend to maintain a stream of air to the upper levels providing room set point and delta T between room set point and the surface temperature of a heat source are maintained at either full- or part-load conditions. ASHRAE Standard 62.1 has acknowledged the promise of superior IAQ offered by displacement ventilation and has assigned a 1.2 ventilation effectiveness (VE) when installed in rooms with ceilings less than or equal to 18 feet.
100% Outside Air Systems
Decoupled hydronic systems should also be given every consideration. ANSI/AHSRAE/ASHE Standard 170 calls out minimum outside air change rates. Continuing a constant exchange of pathogen-free outside air within a room will more effectively flush out airborne particulate and germicides released within that space. This concept is further supported by documents posted on the ASHRAE Epidemic Task Force's (ETF's) website, advancing the concept that increasing ventilation is conducive for maintaining superior air quality. One of the billeted recommendations found at ASHRAE’s ETF website, in its Position Document on Infectious Aerosols (April 2020), states, “Increase outdoor air ventilation and open outdoor air dampers to 100% as indoor and outdoor conditions permit.” Under the site’s health care guidelines in the sub-section titled “Guidance on Recirculation and Increased Outside Air Fraction,” it states: “Evaluate recirculation or increasing outside air fraction from design levels up to 100% based on a specific surge plan.”
The ETF’s position regarding HVAC design in the time of pandemic provides a path forward for improving environmental IAQ. Why would our industry do less than fully evaluate a 100% outside air or dedicated outdoor air system (DOAS) strategies? These systems provide a single pass of outside air through the building without a return air path that would entrain airborne germicides released into a space, allowing for entry into the supply airstream.
Another advantage of 100% outside supply air (OSA) is the energy savings they offer owners by reducing the amount of airflow to health care buildings by delivering only the amount of air that aligns with minimum OSA flow rates in accordance with Table 7.1 of ANSI/ASHRAE/ASHE Standard 170. However, taking ASHRAE’s ETF ventilation recommendations into consideration, DOAS unit airflows can be sized to allow for an increase of outside air that could respond to uncommon events, such as pandemics, or this strategy could be employed during cold and flu season to more effectively flush out buildings at a faster rate to maintain superior IAQ. One-hundred percent OSA systems coupled with other pathogen-mitigating strategies, such as UV light generation and needle point bipolar ionization (NPBI), should be considered as additional effective modalities for germicidal neutralization to create healthier building environments.
 FIGURE 5: A radiant panel layout in a common area at American University, Washington College of Law - Tenley Campus. SmithGroup served as the engineer/architect on this project.
FIGURE 5: A radiant panel layout in a common area at American University, Washington College of Law - Tenley Campus. SmithGroup served as the engineer/architect on this project.100% Outside Air Systems Coupled with Active Chilled Beams (ACBs)
By supplying 100% outside air, these systems will assure the prescriptive minimum of outside air is being delivered to each zone. Depending on how owners wish to operate their facilities in light of ASHRAE's ETF guidance, they may choose to increase air change rates to reduce the risk of spreading infections. ACBs can be designed at more than code minimum flow rates and have historically been designed to be constant volume systems, allowing these devices to maintain discharge air velocities that will promote mixing of space air and room air dilution. Standard ACB models have 2- or 4-pipe configurations, both of which allow for the separation of latent and sensible cooling; however, 4-pipe chilled beam provides tighter thermal comfort control that is conducive to patient well-being and should be given every consideration over a 2-pipe solution.
An alternate take on conventional ACBs is the application of newer displacement ventilation chilled beams, which are low-discharge velocity terminal units mounted low in a wall area. Displacement chilled beams have been gaining attention in school applications and merit a comprehensive look for use in health care environments. They combine the concept of decoupled latent and sensible cooling with thermally stratified air profiles at the occupant zone and above.
100% Outside Air Systems Coupled with Passive Hydronic Terminal Devices
Passive 100% outside air systems offer another layer of environmental enhancement. A passive chilled beam is a sensible cooling-only terminal comprised of a coil horizontally mounted in a ceiling. By supplying chilled water to the beam, sensible heat is removed from the air local to the beam. The cooler air falls into the space via the forces of convection. Ventilation is provided separately from the hydronic terminal device and supplied to the zone by displacement diffusers mounted low in the wall allowing thermal stratification to occur. Heating would occur via a secondary system, such as perimeter baseboard heat. To simplify a passive design, radiant sails or panels could be applied, preventing the need for a secondary heating source, as radiant heating will effectively handle the heating load.
By creating a thermally stratified environment, these systems offer an added layer of protection for safer environments by applying the principles outlined in the aforementioned displacement ventilation narrative.
Conclusion
Mechanical engineers involved in health care design must become intimately familiar with the FGI Guidelines and ANSI/ASHRAE/ASHE Standard 170. These two main publications form much of the framework and building blocks for health care engineering design. Although ANSI/ASHRAE/ASHE Standard 170 provides comprehensive guidelines and serves (in most cases) as minimum code requirements, there is more that can be done to ensure exceptional mechanical designs for our needed institutions that promote the recovery, healing, and general well-being of patients, workers, families, and visitors. As mechanical engineers designing health care projects, we must continually remind ourselves and refocus our efforts to designing spaces that enhance the environment for the occupants of health care facilities. We must do our part to design past the bare minimum, provide better recommendations that raise the level of standard design, and devise ways to design a better environment.
We leave you with the quote: “When a flower doesn’t bloom, you fix the environment in which it grows, not the flower.” Keep this in mind the next time you approach a health care project design or when a client asks you to focus on first costs.
Look for our October 2021 Engineered Systems article, which will take a deeper dive into specific building systems and how proper system selection supports a positive health care built environment.
This article is dedicated to Gina Clarcq for her inspiring contributions.