
FIGURE 1. Typical ambient design conditions.
A hospital with a smart HVAC design can still suffer mold if maintenance misses a beat. Likewise, the best O&M regimen can’t avoid the consequences if the HVAC is designed for the wrong temperature range, or if the humidity level is anyone’s guess. Prevent unwanted condensation and worse with this condensed look at both sides of the IAQ coin.
Two words you do not want to see together in a newspaper headline are “mold” and “hospital.” How dangerous is it and how can you minimize potential mold issues in a hospital?
It is important to understand first that there are no guarantees to yield azeromold growth in a health care facility. After all, as stated in ASHRAE’sHVAC Design Manual for Hospitals and Clinics, “health care facilities are environments of controlled hazards.”1The hazards - molds, bacteria, viruses, etc., - are there. The challenge is to control them to a level that is deemed safe for the facility’s occupants, patients, and caregivers.
In our quest to control these hazards, there are measures that should be considered to minimize the potential for mold growth. For this discussion, these measures are being divided into two categories: design issues and operations issues.
Oftentimes, the root causes of mold-related problems in health care facilities, as well as in any other facility, can be traced back to shortcomings with the initial facility design. These shortcomings often pertain to the building structure itself (the building envelope, the building materials used, etc.).2Other design shortcomings, however, are often related to the HVAC system and its ability, or lack thereof, to control the patient care environment to conditions that are not conducive to mold growth.
Even if all of the bases were covered properly during the design phase, and the facility was built in accordance with the design standards and documents, mold can often still be found in a building because of the way in which the building and its HVAC system are being operated and maintained.
Because the design and operational issues for the health care facility are so numerous, this article will primarily address only those issues that are related to the HVAC system.
How Dangerous Is Mold Growth In The Health Care Facility?
According to the Environmental Protection Agency (EPA), many mold types are very opportunistic and will often infect those people with weakened immune systems (i.e., immuno-compromised individuals).Aspergillus fumigatus, for example, has been known to infect the lungs of immunocompromised individuals. These individuals inhale the mold spores, which start growing in their lungs. Trichoderma has also been known to infect immunocompromised children.3Other health effects can range from simple headaches, sinus, or breathing problems to more severe problems like skin rashes, bleeding of the lungs, cancer, and even death.There is evidence that a direct association exists between exposure to mold and adverse health effects. Mayo Clinic investigators have recently found that inhaled fungus and mold trapped in the nasal mucus are a major cause of sinusitis.4There is also other suggestive evidence that there is an association between exposure to mold and other adverse health effects.5Therefore, it seems only prudent that extra precautions be taken within health care facilities to minimize patient and provider exposure to molds. The following design and operations issues should help in that quest.
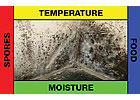
FIGURE 2. Mold square.
Design Issues Contributing to Mold Growth
Many design issues can lead to a lack of moisture control within the hospital that can potentially lead to mold problems. These issues could be building envelope- and construction-related such as poor or improper insulation leading to wall surface condensation. The problems might be improper roof drainage, leaky window and door systems, improper installation of vapor retarders, or any number of envelope-related issues. It might very well be related to having too much water and/or humidity entering the building during the construction phase. However, in the limited scope of this article, the focus is the HVAC system’s design and operation.There are a number of issues that must be resolved before the proper HVAC system can be designed, whether it be intended for the surgical suite, the patient rooms, or the administration offices.
Initially, the proper ambient design conditions must be selected. Too often, only the peak cooling design conditions are considered for sizing the capacity requirements of the system. These ambient conditions are listed in theASHRAE Handbook – Fundamentals as the drybulb temperatures with mean coincident wetbulb temperatures, representing conditions on hot, mostly sunny days. These conditions are used in sizing cooling equipment such as chillers or A/C equipment for cooling control. In some climates, this might be satisfactory; however, in geographic areas known for higher humidity levels, considering only this cooling condition might not be sufficient.
Extreme dewpoint temperature conditions may occur on days with moderate drybulb temperatures, resulting in high relative humidities and peak absolute moisture loads from the weather. These values from tables found in the Fundamentals Handbook are useful for humidity control applications, such as desiccant cooling and dehumidification, cooling-based dehumidification, and fresh air ventilation systems. These values can also be used as a checkpoint when analyzing the behavior of cooling systems at part load conditions, particularly when such systems are used for humidity control as a byproduct of temperature control.6The psychrometric chart for Memphis, TN in Figure 1 highlights what a significant impact the selected ambient extremes can make.
As seen on the chart, if the space were to be maintained at a condition of 75°F drybulb (db) and 50% rh (i.e., 65 grains of moisture/# of dry air [i.e., gr/#], or coincidentally 55° dewpoint), the ventilation air being introduced during the extreme dewpoint condition would require much more dehumidification capacity than the ventilation air at the extreme cooling condition (almost 52% more dehumidification capacity required) just to deliver the ventilation air at a space “neutral” humidity level. Not considering the more difficult peak dewpoint conditions of the ambient air is one of the major reasons that HVAC systems in the hospitals cannot adequately control the humidity during much of the year.
Another reason humidity and condensate problems are being seen in hospitals, particularly within surgical suites, is that the rooms are being kept at cooler conditions than for that which the engineer designed the HVAC system. Most of the time only the general requirements from the American Institute of Architects (AIA) guidelines are considered for the surgical environment’s temperature and humidity range, for example 68°db and 50% rh.
However, nothing in these guidelines shall be construed as precluding the use of temperatures lower than those noted when the patients’ comfort and medical conditions make lower temperatures desirable. Some surgeons may require room temperatures that are outside of the indicated range. All operating room design conditions shall be developed in consultation with surgeons, anesthesiologists, and nursing staff.7The designer must ask the endusers of the facilities what the anticipated space conditions will be.
If the HVAC system had only been designed to maintain the space at the higher room temperatures, then once the room’s temperature is actually lowered (e.g., 60° to 62°db), then the HVAC system’s capacity would very likely not be able to reach the necessary lower absolute moisture levels for the space. If this occurs, the moisture in the air will begin to condense on the cooler surfaces of the ceiling supply air diffusers, the suspended fixtures, and even on the surgical equipment and tables. Condensate raining from the ceiling, after being in contact with the dirt, dust, and mold spores is certain to cause concerns regarding the sterility of the surgical environment.
This same phenomenon can happen in other parts of the hospital as well (e.g., kitchen and dining, labs, even patient rooms); however, the surgical environment is generally the more common area of concern. This is the primary reason the desiccant-based dehumidification systems are becoming much more of a standard in the surgical suites.
Proper selection, sizing, and application of the HVAC systems is essential to ensuring the humidity is controlled to a level to where there is minimal chance the moisture in the air will condense and provide the mold spores with the moisture it needs to flourish. Mechanical HVAC systems (chilled water systems and/or direct expansion [DX] systems) must be selected with the cooling coils capable of supplying air at dewpoints low enough to actually compensate for the moisture gain within the spaces (i.e., latent gain).
For example, if the operating space is to be maintained with a condition of 60° db and 50% rh (i.e., 38.5 gr/#, or 41.3° dewpoint), then a chilled water coil only capable of delivering air off the cooling coils at 50° to 52° (saturated) will not satisfy the need. The supply air would have to be delivered at an absolute humidity level of less than 41.3° dewpoint. This would require either a low temperature chiller or a desiccant-based dehumidification/cooling system.
For a facility only trying to maintain the space at 75° db and 50% rh (i.e., 55° dewpoint), the coils must still be capable of delivering air with a dewpoint less than 55° in order to absorb the space latent gain. If the moisture is not controlled sufficiently by the HVAC system, this could spell disaster with regard to trying to keep significant mold growth out of the facility.
Once the air-handling equipment has been properly sized and selected, care must be taken to ensure that the supply air ducts, the chilled water lines (supply and return) and the refrigerant lines are well insulated. With the cooler air inside the ducts or water inside the chilled water piping, condensation can easily form on the outside of the ducts and/or pipes. The dewpoint temperature of the air surrounding the cooler ducts and pipes could easily be higher than the surface temperature of the ducts and pipes. Condensation will occur when this happens. If the ducts and piping happen to be in the ceiling space, the condensate can drip onto a surface that is loaded with mold food (ceiling tiles, dry wall boards, insulation, plywood, etc.) and all of the necessary elements are there for mold growth.
Once the HVAC system has been selected and properly sized, serious consideration must then be given to the controllability of the systems. As is far too often the case, most HVAC systems are installed with the primary function of either cooling or heating, with the humidity control simply as a secondary function of the system. This is evidenced by the fact that most HVAC systems are installed only with a thermostat installed to operate the system. Including humidity control devices in the controls package for the HVAC system is almost non-existent. How can you control the humidity if it is not even being measured?
Also, far too often, the supply and return air ducts aren’t sealed or insulated properly during construction. On the return side of the equipment, leaky ducts will draw in far more moisture than the cooling coils were designed to remove. The result is a higher than designed and desired humidity level in the space. In an effort to save installation dollars, the return duct is often deleted from the plans and the interstitial space between the suspended ceiling and the roof assembly, or the floor assembly above, is used as a return plenum.
Little thought is given to the fact that this interstitial space is now under a substantial negative pressure and this could cause moisture-laden ambient air to be drawn into the space from an outside wall through cracks and holes if this space is not sealed adequately. This infiltration air is completely unconditioned at this point.
These comments are certainly not meant to be all-inclusive, but simply a starting point for consideration. The HVAC system, the heart and lungs of the facility, must be selected and sized properly for its very important task. And that task is to control the environment to promote the healthiest conditions possible for the patients and the health care providers.
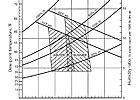
Table 1
O&M Issues Contributing to Mold Growth
Maintaining a clean environment, including a clean HVAC system, will pay great dividends toward minimizing the potential for mold growth (Figure 2). One of the sides of the mold square is that of food. Food for mold spores (anything organic) is generally in abundance within the facility, but there is no reason to spoon-feed the mold spores! Keep the air handlers filters clean, and keep the dust and dirt out of the space as much as possible. If remodeling projects are underway within the hospital, even if it involves simply running new cables above a ceiling system, seal off the construction areas to make certain the airborne debris is unable to get into the areas that should be clean. As a preventative measure, consider engaging the services of an industrial hygienist to assist.Oftentimes in an effort to conserve energy, the chiller is allowed to operate with a slightly elevated leaving water temperature (e.g., elevating from 44° to 46°, possibly). While this will indeed save on the energy bill, and it might be sufficient for keeping the space temperature under control, it could fail miserably at controlling the moisture within the space (especially within the operating rooms). If the humidity within the space should exceed the desired maximum acceptable level (e.g., 55% to 60% rh), then there should be a humidity sensor and transmitter within the space that could override the temperature controls and then lower the chilled water temperature in order to keep the humidity under control.
Building pressurization is a critical factor to monitor in a hospital as it can greatly affect the controllability of the environment. If the building pressure is allowed to become negative due to supply filters being loaded, supply fans running too slow, or return fans running too fast, humid and dirty air can be drawn into the building through cracks and openings. This air is completely unconditioned and can provide several of the necessary ingredients to promote mold growth (e.g., moisture, more spores, and nutrients.) Dynamic pressure differential monitoring must take place in order to ensure the building is under the necessary positive pressure. It would be advisable also to regularly have a TAB evaluation performed on the facility’s HVAC systems.
It is far too common to see water standing in drain pans due to either clogged condensate lines, pans that are not sloped, or drain line connections placed too high above the drain pan’s floor. If there is water standing in the pans, then this water can become a breeding ground for hazardous bacteria and molds. Much of this standing water will also be evaporated back into the supply airstream, saturating the supply duct, making it a prime breeding ground for undesirable hazards.
In conclusion, this article has only highlighted what some might consider the most obvious causes of mold growth, and specifically the lack of control of moisture migrating into the facilities. As obvious as these may seem, these are some of the more common issues found in the design and operation of the health care facilities. Excessive mold growth has been found in too many instances within the facilities that should be the healthiest of them all. Greater attention must be paid, in the design and in the operational phases, to the HVAC system’s capability to actively control the humidity within health care facilities.ES
References
1. American Society of Heating, Refrigerating and Air-Conditioning Engineers.HVAC Design Manual for Hospitals and Clinics,Atlanta, 2003.2. Miller, Dewayne R. and Walter H. Carter, “Solving Water Intrusion and Mold Problems in Tennessee,”EAQP, Inc. & Inspection Center, Inc., December 2002,www.healthyairquality.com.
3. U.S. Environmental Protection Agency.Mold Remediation in Schools and Commercial Buildings, EPA, 402-K-01-001, March 2001:41.
4. The New York Otolaryngology Group.Understanding Sinusitis, 1999, www.newyorksinuscenter.com.
5. Miller, Dewayne R. and Walter H. Carter, Updates on Legislation and Insurance Activity in the United States for “Mould, Asbestos & Lead,”,Healthy Buildings 2003, University of Singapore, December 2003,www.healthyairquality.com.
6. American Society of Heating, Refrigerating and Air-Conditioning Engineers.2005 ASHRAE Handbook – Fundamentals, 2005:28.5.
7. American Institute of Architects.Guidelines for Design and Construction of Hospital and Health Care Facilities, Chapter 7, Table 7.2.
Sidebar: What is Mold?
Molds, mushrooms, mildews, and yeasts are all classified as fungi, a kingdom of organisms. It is estimated that there are between 50,000 and 250,000 species of fungi; however, many of these species have not been classified or named. Fewer than 200 fungal species have been described as human pathogens that cause infections. Multicellular fungi consisting of branching filamentous structures are known as molds.1Of the many mold types, a few seem to be the most common and tend to grab the headlines. Mold types most commonly found in the health care environment areAspergillus,Cladosporium, andPenicillium. While not as common,Stachybotrys, often referred to as black mold2, gets a lot of the attention as well.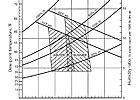
Table 1
How does Mold grow?
There are several factors that contribute to mold growth, and these can best be summarized by what is often referred to as the “mold square.” As seen in Figure 2, it is understood that all four sides of the square must be present in order to foster mold growth. If any of these four elements can be eliminated, mold will not grow.The very genesis of a mold colony is the mold spore … the first side of the mold square. Molds spread and reproduce by making spores, which are small and lightweight, able to travel through air, capable of resisting dry, adverse environmental conditions, and hence capable of surviving a long time.3This can be thought of as the “seed” that germinates. If we could get rid of all of the mold spores in the health care facility, then we would not have a problem. However, the air around us is not sterile and mold spores are abundant in the air outside and inside the facility. Sooner or later a mold spore will land on a surface with a sufficient food source and enough moisture for the spore to germinate.
The second side of the mold square is food. The food sources, or nutrient sources, are also plentiful within the health care environment. Think of the abundance of cellulose enriched materials like grass, leaves, paper, wood, and cardboard products found within and around the facility, not to mention the amount of starches in the wall paper and ceiling tile glues. Like the spores, the food sources are abundant, so this side of the square is readily available within the facility.
Temperature is the third side of the square. If the temperatures within the facility could be maintained outside of the optimal temperature range for mold growth, that could limit the amount of mold found in the health care environment. However, research shows that mold growth generally occurs within the temperature range of about 40°F to 120°. As the human body temperature at 98.6° and the “human comfort zone”4temperatures (Table 1) are well within this temperature range, this side of the square is also satisfied.
The remaining side of the square is themoisture, the only side that can be controlled. Mold amplification indoors is usually due to a moisture problem, which will continue to fuel mold growth. This growth does not require standing water to be present. It can occur when the relative humidity within a space is high. The key to mold control is moisture control. Solve moisture problems before they become mold problems.5
References
1. Centers for Disease Control and Prevention.Mold: Prevention Strategies and Possible Health Effects in the Aftermath of Hurricanes Katrina and Rita, Atlanta, October 2005.2. Miller, Dewayne R., and Walter H. Carter,Molds, Bacteria and other Hazards, EAQP, Inc. & Inspection Center, Inc.,www.healthyairquality.com.
3.ibid.
4. American Society of Heating, Refrigerating and Air-Conditioning Engineers.2005 ASHRAE Handbook – Fundamentals, “Summer and Winter Comfort Zones,” 2005:8.12.
5. U.S. Environmental Protection Agency.Mold Remediation in Schools and Commercial Buildings, 402-K-01-001 March 2001:3.
