The short answer is yes, but the more detailed questions of where and how well have led to a year-and-a-half-long journey that continues.
The obvious concern that differentiates health care facilities from other building types is infection control. With a guiding principle of saving energy while maintaining or improving patient and staff safety, the journey began. In a day-long workshop, a matrix matched health care spaces with the most promising sustainable strategies. Invited to the workshop to critique the proceedings were Andrew Streifel, a recognized infection control expert from the University of Minnesota and officials from California’s Office of Statewide Health and Planning Development (OSHPD). The applications with the greatest possibilities from the workshop were displacement and natural ventilation in patient rooms and public areas. Because natural ventilation is less precise and more difficult to analyze, displacement ventilation became the initial focus. However, parallel research is proceeding on natural ventilation applications.
Traditional overhead ventilation mixes room air from an overhead supply diffuser, ideally creating a homogenous environment throughout the entire room volume. Displacement ventilation supplies cool air low at a low velocity, allowing it to pool across the floor. As the air picks up heat, it rises due to convection in a vertical temperature gradient, ideally in a laminar piston effect.
The goal of displacement ventilation is to condition only the occupied volume and carry contaminants directly up out of the occupied zone without mixing them. Low sidewall displacement ventilation was chosen over raised floor displacement for health care facilities, due to cleanliness concerns. The presumed benefit of displacement ventilation was equal or better environmental comfort and ventilation effectiveness at lower air exchange rates.
When Streifel considered the displacement mechanism for contaminant removal, he was optimistic that it might also have benefits for the control of airborne infectious particles. The formulas for mixing dilution via air exchange rates - applied to overhead mixing ventilation - do not directly apply to displacement ventilation. A hypothesis was created that low sidewall displacement ventilation at lower air exchange rates would be equal to or better than overhead mixing ventilation for environmental comfort, ventilation effectiveness, and airborne particle control. If the hypothesis proved to be true, the energy savings and economic benefits would be dramatic.

figure 1. Patient room.
The Study - Phase I
As Kaiser authorized a research study to test the hypothesis, Mazzetti & Associates became aware that Stantec, an A/E firm in Vancouver, BC, Canada, was planning similar research. The two firms agreed to collaborate on the research and share their findings publicly. Stantec took a holistic look at an emerging best practices hospital, and focused on an outpatient exam room. This space was representative of outpatient diagnostic areas where undiagnosed patients may be present. They evaluated overhead, displacement, and natural ventilation supplemented by radiant heating and cooling.Mazzetti focused on in-patient rooms and emergency waiting rooms. Inpatient rooms were selected, because patients are generally diagnosed and collectively, they represent a significant portion of hospital space. Negative isolation rooms and positive environment rooms were excluded at this time. The emergency waiting room was chosen, as it is one of the areas of highest concern for airborne infection transmission from undiagnosed contagious patients. This article discusses the Mazzetti & Associates portion of the research.

figure 2. Waiting room.
Study Scope
The study included the following elements:- Literature research – to assess prior research to avoid repetition and inform our research
- Mock-up testing – conducted at the test labs of EH Price Company in Winnipeg, MB, Canada
- Field testing – to test both displacement and natural ventilation at the Kaiser Modesto Hospital in California, a new facility available prior to occupancy
- CFD modeling – to corroborate both mock-up and field testing
- Energy modeling – to quantify the energy savings of the sustainable strategies
- Life-cycle costing – to confirm the business case
Mock-up Testing
Testing mock-ups were created for both a patient room and an emergency waiting room at the EH Price Testing Labs in Winnipeg. Figure 1 is a plan of the patient room, which matches the Kaiser template hospital design. Figure 2 is a plan of the emergency waiting room. The 900-sq-ft floor area is about two-thirds of a Kaiser template emergency waiting room, because it is the largest space available at the test labs. Nonetheless, the scale of the room is large enough to test the hypotheses. Parallel mock-up testing was conducted on a medical office exam room under the direction of Stantec.In all cases, overhead ventilation was compared to displacement ventilation at equal or lower air exchange rates. Three yardsticks for comparison were environmental comfort per ASHRAE Standard 55, ventilation effectiveness per ASHRAE Standard 62, and particle control per a qualitative test designed by Streifel.
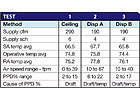
TABLE 1. Patient room environmental comfort.
Environmental Comfort Testing
The ASHRAE Standard 55 test procedure measures sensible temperature, mean radiant temperature and air velocity at six locations and four heights in a space. Using an “operative” temperature, computed from sensible and mean radiant temperatures, and velocity; a “percentage of people dissatisfied” (PPD) is computed. Dissatisfaction can be based on either temperature or draft. ASHRAE Standard 55 stipulates that environmental comfort is satisfactory if the PPD is 20% or less.Tables 1 and 2 summarize results for the patient room and waiting room.
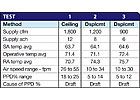
TABLE 2. Waiting room environmental comfort.

figure 3. Temperature profile for a room using overhead
ventilation.
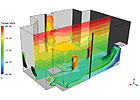
figure 4. Temperature profile for room using displacement ventilation.

TABLE 3. Patient room ventilation effectiveness.
Ventilation Effectiveness Testing
The ASHRAE Standard 62 procedure injects a tracer gas into the supply air and measures the decay over time of the gas concentration in the occupied zone and at the return air. Effectiveness is defined as a ratio of the gas concentration in the occupied zone to the return air, as a measure of how effectively the occupied zone is being ventilated. Thus if there is lack of mixing in overhead supply, the return concentration will be higher due to short circuiting, and the effectiveness will be low. The ratio can exceed 1.0, where the higher the ratio, the better the effectiveness. Anything below 0.80 is unsatisfactory.Tables 3 and 4 summarize results for the patient room and waiting room.

TABLE 4. Waiting room ventilation effectiveness.
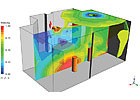
figure 5. Velocity profile for room using overhead ventilation.
Particle Control Testing
Particle testing is a qualitative test to simulate the effects of airborne pathogens introduced into a space via a cough or sneeze and to compare the differences in concentrations and disbursement between conventional and displacement ventilation.Because there is no standardized test for evaluating particle distribution, Streifel and his colleague, Michael Buck, created a procedure they thought would emulate real world airborne pathogen activity. They needed to devise a way to atomize a source into the space, pick a source whose particle sizes would emulate airborne pathogens, and select the proper particle testers to measure the particles. After validating the test procedure at EH Price in Winnipeg, extensive mock-up testing was completed in the Winnipeg test facility for the patient room. Subsequent particle testing was conducted at the Kaiser Modesto Hospital in both the patient room and emergency waiting room.
figure 6. Velocity profile for room using displacement
ventilation.
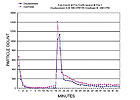
figure 7. Overhead vs. displacement particle concentrations - contagious
provider.
Both Figures 7 and 8 represent the particle concentrations and decay relationships between overhead at 6 ach and displacement at 4 ach. The time-concentration equivalency relationship has been confirmed in repeated mock-up testing and in field testing at the Kaiser Modesto Hospital.
Preliminary Conclusion
It appears that displacement ventilation at lower ach is as good as or better than conventional ventilation at higher ach, considering environmental comfort, ventilation effectiveness, and particle control.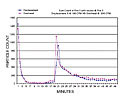
figure 8. Overhead vs. displacement particle concentrations - contagious patient.
Unexpected Observations
Researchers often discover things not directly related to the pursuit of their hypothesis, and our research has been no different. Two noteworthy observations were made regarding the performance of overhead mixing air distribution.Overhead supply simulating displacement. When the patient room mock-up was created in Winnipeg to simulate the Kaiser template layout, a four-way throw diffuser was “inadvertently” used against an interior wall. Air blew against the interior wall, reducing in velocity and increasing in temperature until it pooled onto the floor much like displacement ventilation. This can be seen graphically in Figure 3. It was suspected that this phenomenon caused better than expected ventilation effectiveness (1.24) and lowered the particle concentrations and increased the decay rate. In fact, when the four-way diffuser was moved to the center of the room, particle concentrations increased and decay rates decreased. Ironically, the patient rooms at the Kaiser Modesto Hospital have four way diffusers against interior walls and demonstrated similar performance to the laboratory mock-up.
High emergency waiting room air exchange. AIA Guidelines and Kaiser Standards require 12 ach in emergency waiting rooms to increase the dilution rate for contaminants. For particle testing at the Kaiser Modesto Hospital, the source was a sitting patient near the center of the room. Particles were counted at 3 ft away simulating a person standing nearby and across the room - approximately 30 ft, sitting. While the peak particle counts across the room were lower (approximately 60% of the 3-ft readings), the particles were measured in the same time interval - less than one minute. It raised the question of whether high air exchange rates are beneficial because they dilute pollutants faster or instead are detrimental because they mix and homogeneously deliver airborne pathogens quickly, evenly, and efficiently throughout the room. We will leave this question to other researchers.
Ongoing Research
Research collaboration. This health care ventilation research process is progressing and gaining momentum. As other parties have become aware of this research, a collaborative has emerged. The Healthcare Ventilation Research Collaborative (HVRC) is a group of health care industry professionals with the common goal of promoting improved patient and staff safety and sustainable design in health care facilities through the implementation of innovative engineering concepts that have been thoroughly and scientifically documented. The group includes health care providers, infection control experts, architects, engineers, equipment manufacturers, and affiliated professionals.Displacement ventilation. The HVRC is proceeding with Phase II research, including a more scientifically diligent comparison of overhead and displacement ventilation, with the ultimate goal of modifying accepted design guidelines. Displacement ventilation research will consist of two independent blind components: numerical analysis and empirical analysis. An advisory committee will select researchers for each component, based on their general experience, qualifications, and capability to meet the requirements of a detailed test protocol.
The research will analyze environmental comfort and particle dispersion for a hospital inpatient room, comparing an overhead base case at 6 ach (current accepted minimum) to low sidewall displacement supply at 4 ach. The numerical analysis will look at multiple permutations, varying supply and exhaust locations, and internal and external heat sources. The bedridden patient(s) will be the particle source, simulating regular breathing, a cough and a sneeze. Representative particle concentrations in 2 and 5 micron sizes will be measured at the attendants’ breathing zone and other locations in the room. Environmental comfort will be assessed by measuring four parameters simultaneously: PPDs, ADPI, mean age of air, and air change indices. The empirical analysis will compare only the overhead and displacement base cases as a validation of the numerical analysis. The blind, independent test results will be sealed and submitted to the advisory committee for acceptance and comparison against predetermined deviation criteria.
Optimum displacement ventilation air exchange rates. Pursuant to this research, the numerical model will be utilized to address varying air exchange rates for displacement ventilation. The goal would be to determine the optimum air exchange rates, considering comfort, particle dispersion, and economics.
Emergency waiting room. A separate research project will parallel the inpatient room research to address similar conditions for improving IAQ and efficient ventilation design in an emergency waiting room. Parameters that might be considered in this study include a higher patient and furniture density than a patient room and variable traffic patterns that would affect ventilation strategies.
Natural ventilation. A separate research project will explore the potential of natural ventilation to provide equal or better pathogen dispersal by replicating displacement airflow patterns and/or by flushing rooms with higher air change rates, with further comfort and energy use benefits.ES
