Figure 1. Data shown to reflect antibiotic drug resistance on the increase. (E.
coli is not an airborne bacteria).
While hospitals and health care facilities in the United States are some of the best in the world, the chances of contracting an illness while a pateient in one of these facilities is estimated around 10% of admissions. Several studies and reports estimate that approximately 90,000 people died each year as a result of hospital-acquired infections (HAI), also commonly called nosocomial infections. While many of these nosocomial infections are acquired through other than the airborne route, there is solid evidence that inhalation of bacteria and viruses in hospital air can and does cause many additional patient problems.
In 2005, the Pennsylvania Health Care Cost Containment Council (PHC4) issued a research brief that detailed the cost and quality implications of HAI in Pennsylvania. The report examined reports of nosocomial infections by the billing of the insured, both public and private, and found some staggering data. There were some 11,668 HAIs from 1,562,600 admissions to the state’s 173 general acute care hospitals. These HAI cases lead to additional per person average charges of $160,305, vs. $32,000 without infections, 15.6 additional days in the hospital, and a staggering $2 million in additional hospital charges. Costs aside, there were 12.8% more mortalities of those infected vs. 1.1% of those without infections.
Hospitals air tends to provide an indoor environment that may have increased levels of virus and bacteria that a patient might merely inhale in order to become infected. Add to this that by their very nature, patients already may have other risk factors for developing complications.
Antibiotics are currently being dispensed more frequently and the resistance to many types of antibiotics is on the rise (Figure 1). The recent news about Andrew Speaker who traveled into the United States with what is known as extensively drug-resistant tuberculosis (XDR-TB) involved but one of many types of bacteria that have become resistant to the all mainline antibiotics (and three to six secondary types).
Not only are we becoming more resistant to antibiotics, but this drug resistance is also transmissible to other people. Because bacteria and viruses can be contracted via the airborne route, this offers an opportunity for much better air cleaning and air management in hospitals and health care facilities than is current practice. Included in the scope of health care facilities are outpatient facilities and doctor’s offices - commercial buildings built to accommodate commercial offices - that are now increasingly being used for outpatient surgery. Most of these types of facilities have standard rooftop HVAC systems with MERV 4 or MERV 6 filters, providing neither the level of air cleanliness nor air patterns needed for best-practice patient care.
So what can hospitals and health care facilities do to decrease patient exposure to contaminants in the air without expending money? Here are some cost-effective, energy saving alternatives to the current practice.
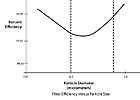
Figure
2. Filter efficiency vs.
particle size.
We continue to hear engineers say that HEPA filters do not remove smaller ultrafine contaminants such as viruses. This is incorrect. HEPA filters do remove particles below 1 micrometer (Figure 2) in which viruses and ultrafine particles exist. Also, many viruses piggyback on droplet nuclei and can be effectively and efficiently removed by HEPA filtration or even MERV 14 and15 filtration.
Emergency room(ER).The ER continues to be a potential source of large amounts of contaminants and infectious agents from people awaiting diagnosis and treatment. These areas must be filtered at MERV 14 levels with higher air exchange rates, air pressure negative to surrounding space, and laminar flow air management per theAmerican Institute of Architects (AIA) Guideline. TheGuidelinerecommends 12 ach with 2 ach from outdoor air with all air exhausted to the outdoors. By its own statement, the AIA knows the value of air cleaning. It states,“… for airborne infection control, air may be recirculated within individual isolation rooms if HEPA filters are used.”1

Figure 3. Airflow pattern moving and removing contaminants away from patient.
es0707-veeck-guestcolumn-fig3-lg.jpg
So why dump all of this air from the ER outdoors? Effective filtration using MERV 14 filters and recirculating this air can save re-heating and re-cooling costs. Adding in-room portable HEPA air cleaners can supplement the overall cleanliness on an ongoing basis, provide better air movement to prevent one patient from infecting another, and would be in place and available in case of an extraordinary outbreak of a highly infectious event.Patient rooms. The AIA recommends 6 ach in patient rooms. While this is adequate for comfort, more air exchanges using contaminant removal air patterns in patient rooms (Figure 3), which do not have to employ HEPA filtration, can help provide a cleaner environment. The use of MERV 14 or better filters can efficiently accomplish this cleaning.
In addition, exhaust from toilets and other non-contaminated rooms, which now is fully exhausted to the outdoors, can safely be run through particle and molecular filtration and supplied back as return air, saving energy costs.
In summary, there are additional ways that hospital and health care facility can provide a complete wellness program for patients. Better management of air and air filtration as a health/safety technology that cleans contaminants from the air will help reduce the chances of airborne nosocomial illness and save lives, energy costs, and health care costs.ES